Abstract
Several countries are in different phases of safely lifting the lockdowns necessitated by the Covid-19 pandemic and re-opening their economies. As they do so, it is important for authorities to recommend or impose some public health measures like social distancing and wearing face masks. Scientific articles are appearing in peer reviewed medical journals and even in the lay press on this topic. Some of the scientific definitions used in these articles might be erroneous. It is therefore necessary for the scientific community to highlight these errors, so as not to convey the wrong meaning. The purpose of this article is to highlight the importance of correct usage of scientific definitions. Scientific definitions of basic reproduction number (R0), effective reproduction number (Re) and herd immunity are necessary to correctly understand the epidemiological basis for measures to control the COVID-19 outbreak. R0 is defined as expected number of secondary cases produced by a single (typical) infection in a completely susceptible population. R0 is essentially the ratio between transmission rate and recovery rate. The transmission rate in turn is determined by the rate of contacts in the host population and the probability of infection being transmitted during the contact. Recovery rate is a reciprocal of duration of infectiousness. Re is defined as expected number of secondary cases produced by a single infection in a population that is made up of both susceptible and non-susceptible hosts. Re is given by the formula: Re= R0 · (S/N), where S is the number of “susceptible” individuals and N is the total number of all individuals, i.e. susceptible, exposed, infected, and recovered. Herd immunity (actually ‘herd protection’) occurs when a significant proportion of the population is immune by some mechanism, usually by vaccination, resulting in protection for susceptible individuals who are not immune. Care must be taken not to use R0 and Re interchangeably as they have distinct implications with regard to control measures. Relying on herd immunity without vaccination is not a scientific solution in these circumstances.
Keywords
COVID-19, Epidemiology, Basic reproduction number, Effective reproduction number, Herd immunity, Community transmission, Face shields, Universal airborne precautions
Commentary
As a part of public health measures to contain corona virus disease 2019 (COVID-19), several countries have imposed lockdown restrictions which resulted in unstable economies. Now, the world is preparing to find different solutions to open up the economy while simultaneously containing the COVID-19. In this regard, a few concepts like, “basic reproduction number” (R0), “effective reproduction number” (Re) and “herd immunity” applicable for any infectious disease outbreaks are important. A clear scientific definition of R0, Re and herd immunity may be worth revisiting, to correctly understand novel proposals suggested to control the COVID-19 outbreak. The difference in the definitions are so subtle that it may miss the attention of rigorous peer review process and careful scrutiny of editorial boards of even reputed journals. For example, a recent publication highlighted the misuse of the term ‘rate’ as in case-fatality rate in publications related to COVID-19 [1]. The scientific definition of the term ‘rate’ has a notion of time and should not be used in cross-sectional studies. Again, in another related publication, the issue of wrong assumptions for distribution of COVID-19 incidence rates with ‘binomial’ or ‘normal’ instead of ‘Poisson’ distribution for computation of confidence intervals was brought out [2]. The aim of this article is to highlight the importance of correct usage of scientific definitions related to R0, Re and ‘herd immunity’.
A recent publication discussed the issue of potential use of face shields in the community for containment of COVID-19 [3]. In their narration, the authors defined R0 as “effective reproduction number” when it should have been “basic reproduction number”. In the modelling with SEIR, i.e., Susceptible, Exposed, Infected, Recovered, two parameters R0 (basic reproductive number) and Re (effective reproductive number) give us information about the effectiveness of control measures (Table 1) [4,5]. Both R0 and Re are dimensionless numbers and exclude new cases produced by secondary cases. For example, a similar SIR modeling was used to illustrate the dynamics of the coronavirus pandemic in Italy and make some global predictions [6]. The zero in “R0” means that it is estimated when there is zero immunity in the population even though not everyone will necessarily be susceptible to infection.
|
Item |
R0 |
Re |
|
Conceptual definition |
Expected number of secondary cases produced by a single (typical) infection in a completely susceptible population |
Expected number of secondary cases produced by a single (typical) infection in a population that is made up of both susceptible and non-susceptible hosts |
|
Formula for key determinants |
Ratio between transmission rate and recovery rate* |
Re= R0 · (S/N) † |
|
Value <1 |
Spread of infection in the population unlikely |
Outbreak will not be sustained |
|
Value =1 |
Sharp threshold between the disease dying out or causing an epidemic |
Infection will be endemic |
|
Value >1 |
Infection will be able to start spreading in a population |
Outbreak propagates |
|
* The transmission rate in turn is determined by the rate of contacts in the host population and the probability of infection being transmitted during contact. Recovery rate is reciprocal of duration of infectiousness †Where S is the number of “susceptible” individuals and N is the total number of all individuals, i.e. susceptible, exposed, infected, and recovered |
||
Current estimates of R0 for COVID-19 are believed to be about 2·2 [7] and can range from 2 to 3. With the estimate of 2.2 for R0, if 80% of the population is susceptible, then Re will be 1.76, (2.2 x 0.8). The Re can be reduced by reducing the number of susceptible individuals. Obviously, the number of susceptible individuals will be reduced by an increased pool of recovered patients with protective natural immunity or by vaccination. The R0 can be reduced by public health measures such as social distancing with lockdown, preventing congregations, mass gatherings and similar interventions including the use of face shields. The rationale for using face shields is that infection can be transmitted via respiratory droplets (>5 μm), aerosols (≤ 5 μm) or submicron aerosol (<1 μm) exhaled from infected individuals. Submicron virus-containing aerosols can be transferred deep into the alveolar region of the lungs, where immune responses seem to be temporarily bypassed [8]. In an open letter to the WHO, 239 scientists from 32 countries have claimed that the Covid-19 coronavirus is airborne [9]. This issue of potential aerosol transmission is of serious concern during presymptomatic/asymptomatic stage [10]. Hence, face shields can potentially reduce transmission in the community setting. The implicit goal of face shields alone or in combination with other non-vaccination interventions is to interrupt transmission by reducing the R0 to less than 1. The face shields attempt to reduce the transmission rate, but they have no effect on the recovery rate. Obviously, face shields do not increase the immune status of the population. Hence, the authors proposing the face-shield solution were actually referring to “basic reproduction number”, R0, not the “effective reproduction number”, Re, in the context of their narration [3].
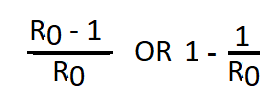
Another important aspect in the present context is “herd immunity” as there is an indication that some policy makers are relying on it as a solution to go hand-in-hand while opening up their economies. For example, some policy makers even suggested that the detection of antibodies to COVID-19 could serve as the basis for an “immunity passport” or “risk free certificate” that would enable individuals to travel or to return to work. However, such a concept did not get the support from the World Health Organization. Herd immunity occurs when a significant proportion of the population is immune by some mechanism, resulting in protection for susceptible individuals who are not immune. Herd immunity is actually ‘herd protection’ from scientific standpoint as it gives protection to vulnerable population. The herd immunity threshold is the proportion of a population that needs to be immune in order for an infectious disease to become stable in that community and is given by the formula [11]
Thus, with the current estimate of R0 for COVID-19 being about 2.2, the herd immunity threshold will be 54.5%. If the threshold for herd immunity is surpassed, then Re will be <1 and the epidemic will not be sustained. This is an important measure used in immunization programs with a primary aim to eradicate the infection. At present without vaccination, immunity can be expected only by recovery from infection. In other words, that proportion of the population according to the estimate for R0, 54.5% should get infected and then recover with protective immunity (IgG seroconversion) to achieve herd immunity. In addition, such a strategy will put several vulnerable people at risk for serious complications of the infection including mortality. A recent review indicated that recovery from COVID-19 might confer immunity against reinfection, at least temporarily, but several questions remain unanswered [12]. The essential questions are: Does immunity occur after recovery from COVID-19 infection?; why some patients seem not to develop humoral immune response?; what is the durability of neutralizing antibodies?; does robust IgG response correspond with immunity?. A recent, nationwide, population-based seroepidemiological study showed that the seroprevalence was 5% (95% confidence interval, 4.7 to 5.4). Spain is one of the European countries most affected by the COVID-19 pandemic [13]. An accompanying commentary stated that any proposed approach to achieve herd immunity through natural infection is not only highly unethical, but also unachievable [14]. Hence, relying on herd immunity conferred only by natural immunity is not a scientific approach.
In summary, scientific definitions of R0 and Re should be noted and care must be taken not to use them interchangeably as they have distinct implications with regard to control measures for the COVID-19 outbreak and attempts to reopen the hampered economies. Relying on herd immunity without vaccination is not a scientific solution in these circumstances.
Conflicts of interest
The author declared no conflicts of interest
Author’s Contribution
Srinivas Mantha, MD: This author conceived the idea and written and finalized the manuscript.
Acknowledgments
Authors thank Venkat R Mantha, MD, FFARCSI, Anesthesiologist, Houston, TX for thoughtful comments on the manuscript.
References
2. Tarantola A, Gautier L. Biostatistics to better detect fishy findings. The Lancet Infectious Diseases. 2020 Jun 29.
3. Perencevich EN, Diekema DJ, Edmond MB. Moving personal protective equipment into the community: face shields and containment of COVID-19. JAMA 2020; 323(22):2252-53
4. Ridenhour B, Kowalik JM, Shay DK. Unraveling r 0: Considerations for public health applications. American Journal of Public Health. 2018 Dec;108(S6):S445-54.
5. Pandit JJ. Managing the R0 of Covid‐19: mathematics fights back. Anaesthesia. 2020 May 28.
6. Nesteruk I. Dynamics of the coronavirus pandemic in Italy and some global predictions. Journal of Allergy and Infect Diseases. 2020;1(1):5-8.
7. Altmann DM, Douek DC, Boyton RJ. What policy makers need to know about COVID-19 protective immunity. The Lancet. 2020 May 16;395(10236):1527-9.
8. Prather KA, Wang CC, Schooley RT. Reducing transmission of SARS-CoV-2. Science. 2020 May;368(6498):1422-24
9. 239 Experts with One Big Claim: The Coronavirus Is Airborne. https://www.nytimes.com/2020/07/04/health/239-experts-with-one-big-claim-the-coronavirus-is-airborne.html (Accessed on 7/7/2020)
10. Oran DP, Topol EJ. Prevalence of Asymptomatic SARS-CoV-2 Infection: A Narrative Review. Annals of Internal Medicine. 2020 Jun 3.
11. Fine P, Eames K, Heymann DL. “Herd immunity”: a rough guide. Clinical Infectious Ddiseases. 2011 Apr 1;52(7):911-6.
12. Kirkcaldy RD, King BA, Brooks JT. COVID-19 and Postinfection Immunity: Limited Evidence, Many Remaining Questions. JAMA. 2020 Jun 9;323(22):2245-6.
13. Pollán M, Pérez-Gómez B, Pastor-Barriuso R, Oteo J, Hernán MA, Pérez-Olmeda M, et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. The Lancet. 2020 Jul 6.
14. Eckerle I, Meyer B. SARS-CoV-2 seroprevalence in COVID-19 hotspots. The Lancet. 2020 Jul 3.