Abstract
Nutritional status is a sensitive indicator of health. There is not a single parameter that serve as the only and best parameter to evaluate malnourished patients or patients with risk for malnutrition. Patients with oral squamous cell carcinoma were a focus of concern for nutritional impairment. Nutritional impairment is a common phenomenon among the patients with oral squamous cell carcinoma. But it is often ignored in treatments and follow-up care. The objective of the study was to assess relationship between lymphocyte and wound dehiscence of patients with oral squamous cell carcinoma. Sixty oral squamous cell carcinoma patients were histologically confirmed. This study was descriptive and cross-sectional study. All patients were studied and followed until discharge from hospital. Surgery of primary lesion with neck dissection were performed for all patients under general anesthesia. The mean age was 47.6 ± 10.8 years in group I, 49.7 ± 8.6 years in group II. Regarding the total lymphocyte count of the patients, it was found that 32 (65.3%) patients had normal nutrition in group I and 5 (45.5%) moderate malnutrition in group I. The mean total lymphocyte count was found 1020.0 ± 819.1 mm3 in group I, 1736.0 ± 474.8 mm3 in group II. The mean total lymphocyte count was statistically significant (p<0.05) between the two groups.
Keywords
Total lymphocyte count, Wound dehiscence, Oral squamous cell carcinoma
Introduction
Patients with oral squamous cell carcinoma were one of the focused areas of concern for malnutrition. Oral squamous cell carcinoma directly impairs oral intake and the increasingly intensive treatments magnify the risk for severe malnutrition. Antineoplastic therapy not only contribute to local disease control and survival, but also create and exacerbate multiple symptoms that further compromise oral intake. Oral squamous cell carcinoma patients often require non-volitional feeding [1-3]. Unlike simple malnutrition, cancer patients’ negative energy balance and profound skeletal muscle wasting was driven by a combination of reduced food intake and abnormal metabolism. Nutritional status impairment was reported frequently in oral squamous cell carcinoma patients. The previous studies had shown, a clear relationship between nutritional deficit and morbidity. Most of these studies reported that malnutrition to be present in 35% to 50% of all oral squamous cell carcinoma patients [4-9]. Aghdaii et al. [10] shown significance of pre-operative TLC as a prognostic criterion of surgery and shown that TLC<1500 cells/mm3 was associated with significantly high mortality and morbidity. Low TLC was associated with more frequent post-operative wound dehiscence.
Materials and Methods
This cross-sectional study was carried out from 1st January 2014 to 31st December 2014 in Oral & Maxillofacial Surgery Department, Bangabandhu Sheikh Mujib Medical University, Shahbag, Dhaka, Bangladesh and consecutively Dhaka Dental College in Oral & Maxillofacial Surgery Department, Dhaka Dental College & Hospital, Dhaka, Bangladesh. Admitted-patients visiting the study places were used as the study population. Regarding nutritional status, a TLC of >1800 mm3 was considered as normal nutrition, 1500-1800 mm3 was considered as mild depletion; 900-1500 mm3 as moderate depletion; and <900 mm3 as severe depletion [11]. The patient samples of 60 consecutive patients diagnosed with oral squamous cell carcinoma were served as cases. The cases were assigned to sub categories based on their matched inclusion criteria. The samples were collected after obtaining institutional review board approval and with their informed consent. In this study, 60 patients presenting with oral squamous cell carcinoma were selected. Data were collected through a structured data collection sheet including questionnaire. A sample of such data collection sheet was attached. Data were collected by the researcher himself in close supervision of the guide. The participants were histologically confirmed oral squamous cell carcinoma patients. They received surgery, radiotherapy, chemotherapy or a combination of these as per necessity. Stratified sample design was applied after interviews, clinical examinations, and simultaneous investigations by the doctor. All patients were studied followed until discharge from hospital. Surgery of primary lesion with neck dissection were performed in case of all patients under general anesthesia. The patients were operated under general anesthesia post-operatively were maintained by nasogastric tube until 7 days. Postoperative complication was wound dehiscence. Patients were undergone for total maxillectomy/ mandibulectomy should be examined clinically until 7 days. In all patients, swallowing was started 8-12 days postoperatively, by drinking water, and gradually extended to a complete diet.
Results
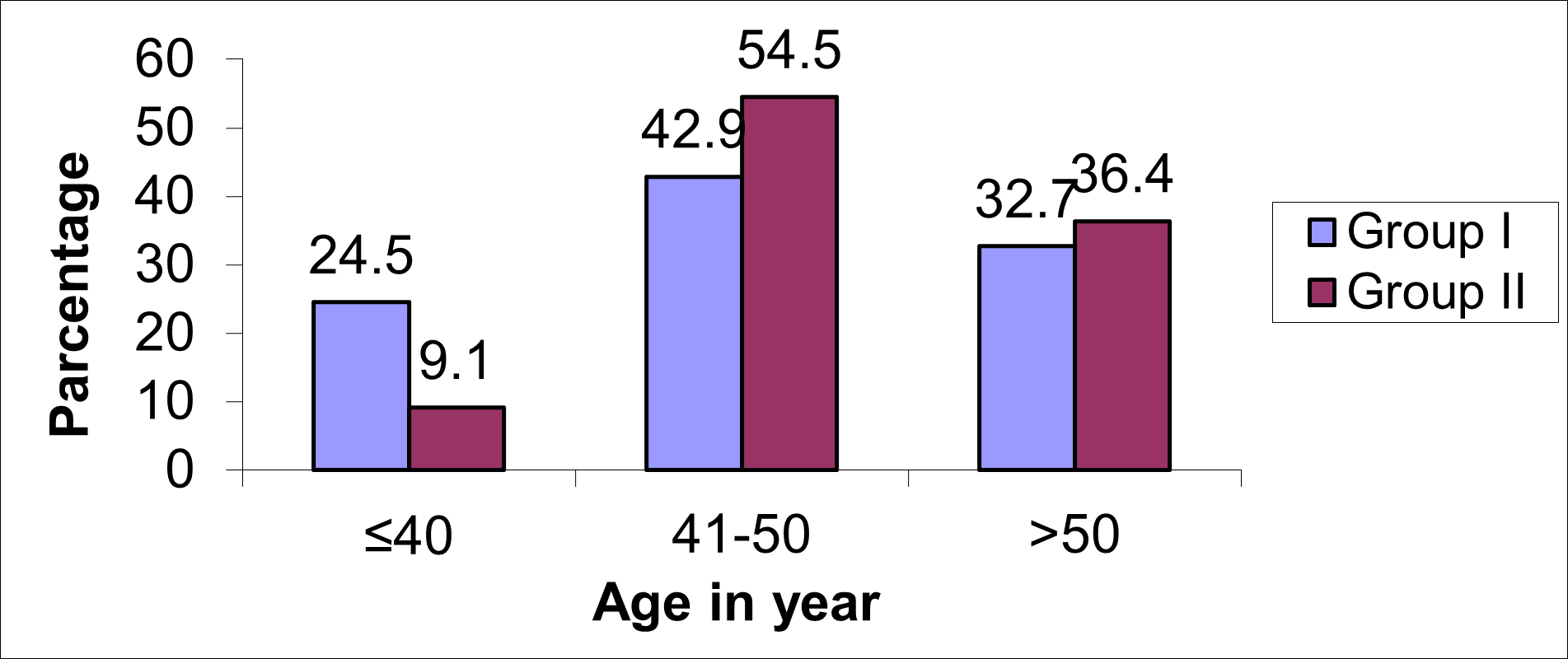
Regarding the age of the patients, it was found that the majority (42.9%) patients were aged 41-50 years in group I and 6 (54.5%) patients in group II. The mean age was found to be 47.6 ± 10.8 years in group I and 49.7 ± 8.6 years in group II. The mean age was not statistically significant (p>0.05) between the two groups (Figure 1).
Figure 1. Age distribution of the study patients.
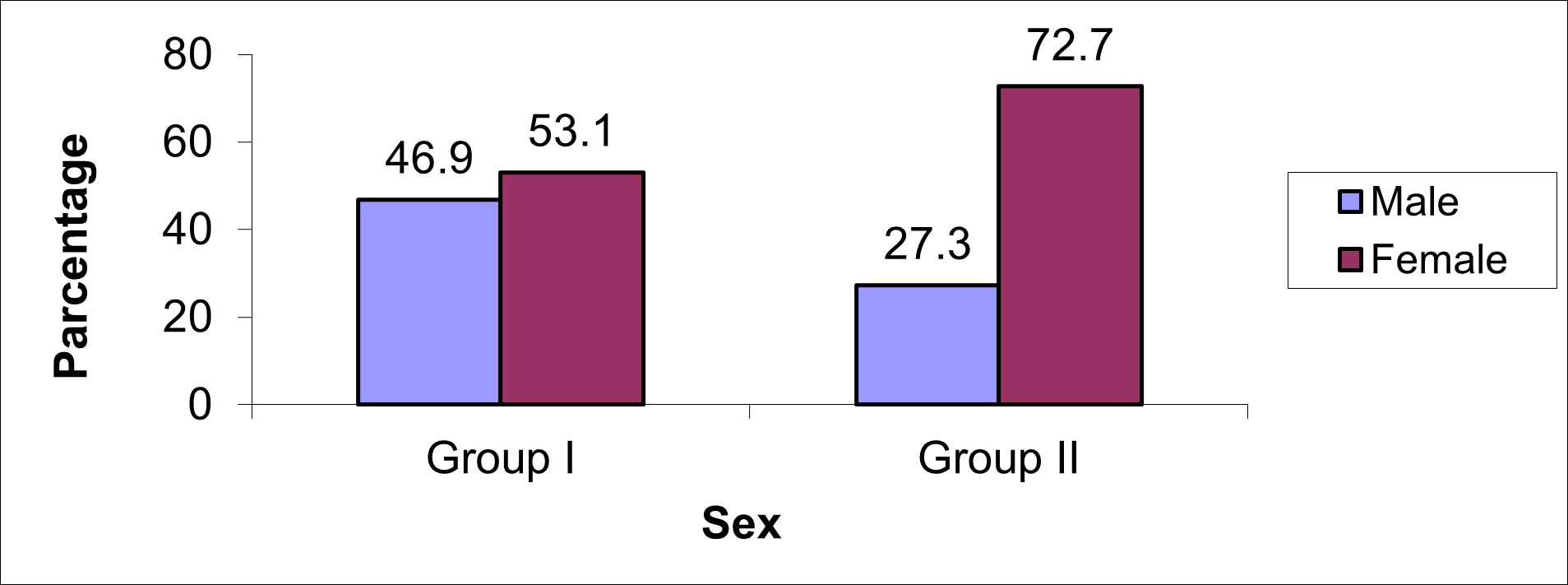
Regarding the sex of the patients, it was found that majority (53.1%) patients were female in group I, 8(72.7%) and male in group II. The difference was not statistically significant (p>0.05) between the two groups (Figure 2).
Figure 2. Sex distribution of the study patients.
Regarding the total lymphocyte count of the patients, it was found that 32 (65.3%) patients had normal nutrition in group I and 5 (45.5%) had moderate malnutrition in group I (Table 1). The mean total lymphocyte count was found to be 1020.0 ± 819.1 mm3 in group I, 1736.0 ± 474.8 mm3 in group II. The mean total lymphocyte count was statistically significant (p<0.05) between the two groups.
|
Total lymphocyte count (mm3) |
Group I (n=49) |
Group II (n=11) |
p value |
||
|
|
n |
% |
n |
% |
|
|
>1800 (Normal nutrition) 1500-1799 (Mild malnutrition) 900-1499 (Moderate malnutrition) |
32 15 2 |
65.3 30.6 4.1 |
3 3 5 |
27.3 27.3 45.5 |
|
|
Mean ± SD |
2282.6 ± 819.1 |
1736.0 ± 474.8 |
0.037s |
||
|
Range (min-max) |
1020.0-4972.0 |
1300.0-2711.0 |
|||
Discussion
Nutritional impairment is reported frequently in oral cancer patients. In previous studies, a clear relation between nutritional deficit and morbidity had been shown. Most of these studies reported malnutrition to be present in 35% to 50% of all oral cancer patients [4-9]. The importance of nutrition on maxillofacial surgery was first recognized in 1930s, when surgical outcomes were noted to be adversely affected by malnutrition. In 1936, Cuthbertson’s descriptions of the adverse effect of malnutrition on his patients made surgeons aware of this relationship. Although this connection was recognized, there was little to be done for hospitalized patients for the next 30 years. Oral squamous cell carcinoma is becoming a prevalent disease in all study age groups especially in our population. Surgery is the treatment of choice for most cancer patients. Change in nutritional status is associated with reduced organ function and deterioration of immune status. The presence of a chronic inflammation, as observed in cancer for instance, increases catabolism and greatly alters immune defenses [12]. Various studies have highlighted a correlation between malnutrition and post-operative complications in oral cancer patients, in the specific context of surgery where an altered nutritional status is associated with increased surgical morbidity and mortality. Nutritional assessment is currently recommended, particularly in situations where nutritional deficit is associated with an increased risk of complications. Keeping these points in mind, this study was conducted to assess nutritional status and their relationship to post-operative wound dehiscence in oral squamous cell carcinoma patients to a satisfactory level. The study was performed as cross-sectional and conducted in Oral and Maxillofacial Surgery Department, BSMMU and Dhaka Dental College and Hospital. In this study regarding the total lymphocyte count (TLC) of the patients, it was found that 32 (65.3%) patients had normal nutrition in group I and 5 (45.5%) had moderate malnutrition in group I. The mean total lymphocyte count was found to be 1020.0 ± 819.1 mm3 in group I and 1736.0 ± 474.8 mm3 in group II. The mean total lymphocyte count was statistically significant between the two groups. Aghdaii et al. showed significance of pre-operative TLC as a prognostic criterion in surgery and found that TLC<1500 cells/mm3 was associated with significantly high morbidity. In hospital wound dehiscence was 28.4% with TLC <1500 cells/mm3. Jensen et al. [13] showed complications related to surgeries performed on malnourished patients. They found 59% post-operative complications developed on TLC<1000 cells/mm3. Regarding the age of the patients, it was found that the majority (42.9%) patients were aged 41-50 years in group I and 6 (54.5%) patients were aged 41-50 years in group II. The mean age was found to be 47.6 ± 10.8 years in group I and 49.7 ± 8.6 years in group II. The mean age was not statistically significant between the two groups. Regarding the sex of the patients, it was found that majority (53.1%) patients were female in group I and (72.7%) male in group II. The difference was not statistically significant between the two groups. From the current study it has been observed that all parameters of nutritional status were related to wound dehiscence. In the past, numerous studies have demonstrated various parameters as nutritional parameters. The sample size of the study was relatively small, which is the main limitation of our study. Malnutrition is directly related to post-operative wound dehiscence. So, nutritional status for every cancer patient should be assessed pre-operatively because preoperative nutrition may reduce post-operative complications (wound dehiscence). Further studies are needed in future to investigate whether it is possible to counteract the adverse effects of malnutrition on surgery by preoperative nutritional support.
Conclusion
The findings of this study may have a major impact on surgical strategies in the future, because pre-operative nutrition might reduce postoperative complications in the patient group. Regarding the total lymphocyte count of the patients, it was found that 32 (65.3%) patients had normal nutrition in group I. The mean total lymphocyte count was found to be 1020.0 ± 819.1 mm3 in group I and 1736.0 ± 474.8 mm3 in group II. The mean total lymphocyte count was statistically significant between the two groups. Further studies are needed in future to investigate whether it is possible to counteract the adverse effects of malnutrition on surgery by preoperative nutritional support.
References
2. van den Berg MG, Rasmussen-Conrad EL, van Nispen L, van Binsbergen JJ, Merkx MA. A prospective study on malnutrition and quality of life in patients with head and neck cancer. Oral Oncol. 2008 Sep;44(9):830-7.
3. Jager-Wittenaar H, Dijkstra PU, Vissink A, van der Laan BF, van Oort RP, Roodenburg JL. Critical weight loss in head and neck cancer--prevalence and risk factors at diagnosis: an explorative study. Support Care Cancer. 2007 Sep;15(9):1045-50.
4. Brookes GB. Nutritional status--a prognostic indicator in head and neck cancer. Otolaryngol Head Neck Surg. 1985 Feb;93(1):69-74.
5. Hussain M, Kish JA, Crane L, Uwayda A, Cummings G, Ensley JF, et al. The role of infection in the morbidity and mortality of patients with head and neck cancer undergoing multimodality therapy. Cancer. 1991 Feb 1;67(3):716-21.
6. Matthews TW, Lampe HB, Dragosz K. Nutritional status in head and neck cancer patients. J Otolaryngol. 1995 Apr;24(2):87-91.
7. Linn BS, Robinson DS, Klimas NG. Effects of age and nutritional status on surgical outcomes in head and neck cancer. Ann Surg. 1988 Mar;207(3):267-73.
8. Bassett MR, Dobie RA. Patterns of nutritional deficiency in head and neck cancer. Otolaryngol Head Neck Surg. 1983 Apr;91(2):119-25.
9. Westin T, Ahlbom E, Johansson E, Sandström B, Karlberg I, Edström S. Circulating levels of selenium and zinc in relation to nutritional status in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg. 1989 Sep;115(9):1079-82.
10. Aghdaii N, Ferasatkish R, Mohammadzadeh Jouryabi A, Hamidi SH. Significance of preoperative total lymphocyte count as a prognostic criterion in adult cardiac surgery. Anesth Pain Med. 2014 Jun 23;4(3):e20331.
11. Gottschlich MM, Matarese LE, Shronts EP. Nutrition support dietetics: core curriculum. American Society for Parenteral & Enteral Nutrition; 1993.
12. Bhuiyan AK, Kabir MJ, Rahman MM. Nutritional Indicators for Postoperative Morbidity in Elective Oncological Surgery. Journal of Surgical Sciences. 2012;16(1):3-10.
13. Jensen GL, Mirtallo J, Compher C, Dhaliwal R, Forbes A, Grijalba RF, et al. Adult starvation and disease-related malnutrition: a proposal for etiology-based diagnosis in the clinical practice setting from the International Consensus Guideline Committee. JPEN J Parenter Enteral Nutr. 2010 Mar-Apr;34(2):156-9.