Abstract
Introduction: Leiomyomas are benign smooth muscle tumors most commonly originating from the uterus, but on rare occasions, they can develop in extra-uterine sites. Such atypical presentations may complicate preoperative diagnosis, particularly when mimicking other adnexal pathologies. We report a rare case of an ovarian leiomyoma presenting as an acute abdomen, highlighting the diagnostic and surgical challenges encountered.
Case Description: A reproductive-aged woman presented with sudden-onset severe lower abdominal pain and clinical features consistent with an acute abdomen. Imaging revealed an adnexal mass with features suggestive of ovarian torsion. Emergency laparotomy identified a solid mass inseparable from the ovary. Salpingo-oophorectomy was performed. Gross and histopathological examination confirmed the diagnosis of an ovarian leiomyoma with torsion.
Conclusion: Although ovarian leiomyomas are rare, they should be considered in the differential diagnosis of solid adnexal masses, especially in cases presenting with acute abdomen. Preoperative differentiation from other ovarian tumors is challenging, and definitive diagnosis relies on histopathology. Prompt surgical intervention remains crucial to prevent complications related to torsion and ischemia.
Keywords
Leiomyoma, Acute abdomen, Parasitic leiomyoma
Introduction
Uterine fibroids are benign, monoclonal tumors originating from the smooth muscle cells of the uterine wall and represent one of the most common gynecological neoplasms in women of reproductive age [1]. They are found during the middle and later reproductive years where it affects one in five women [1–3].
Parasitic myomas are uncommon variants of leiomyomas that develop when a pedunculated subserosa fibroid becomes detached from the uterus, loses its original vascular supply, and establishes a new blood source from surrounding organs [4–6]. They can also arise following gynecological procedures involving tissue fragmentation, such as power morcellation during laparoscopic surgery. In the FIGO leiomyoma classification system, they are categorized as type eight [6]. Historically considered rare since their first documentation in the early 20th century, the reported frequency has risen in parallel with the increased use of minimally invasive surgery and morcellation devices [5–7]. While most cases are linked to iatrogenic causes, the present case appears to have originated spontaneously from pelvic mesenchymal tissue, representing a de novo occurrence rather than one secondary to prior surgical intervention [5,7]. This case of parasitic fibroids was written to illustrate the diagnostic dilemma that may be encountered in women with acute abdomen with no prior symptoms suggestive of leiomyoma.
Case Presentation
A 36-year-old woman presented during menstruation with severe, acute lower abdominal pain of 24 hours’ duration, unrelieved by parenteral analgesics. She had no prior history of dysmenorrhoea or menorrhagia and was under evaluation for an abdominal mass at another private clinic.
Past medical and gynecological history
She reported no significant past medical history. There was no history of prior abdominal surgery. She had regular menstrual cycles and no previous gynecological complaints.
Investigations
Previous workup at the private clinic had included serum tumor markers, which showed normal carcinoembryonic antigen (CEA), lactate dehydrogenase (LDH), alpha-fetoprotein (AFP), and human chorionic gonadotropin (HCG) levels, with a marginal elevation of cancer antigen 125 (CA-125). She had not yet undergone the requested abdominopelvic ultrasound scan. On admission to our facility, full blood count, serum electrolytes, urea, and creatinine were within normal limits. Bloodborne virus screening and serum pregnancy test were negative.
Examination
On physical examination, she appeared in severe painful distress. Abdominal examination revealed a palpable, mobile mass in the left lumbar region with marked tenderness. Vital signs were as follows: respiratory rate 26 cycles/min, heart rate 100 beats/min, blood pressure 130/70 mmHg, and oxygen saturation 97% on room air.
Imaging
Urgent abdominopelvic ultrasonography demonstrated marked probe tenderness over the left iliac region and a 12 × 8 cm mass extending from the left lumbar area to the left iliac fossa, separate from the uterus. The left ovary was not visualized distinctly from the mass. A presumptive diagnosis of ovarian torsion was made, with torsion of a pedunculated fibroid considered as a differential.
Abdominopelvic CT scan done revealed a left adnexa mass measuring 14 × 10 cm with a non-vascular pedicle attached to the fundus of the uterus.
Management and outcome
The patient was counseled and taken for emergency laparotomy. Intraoperative findings revealed a double-twisted torsion of a 12 × 8 cm irregular, solid left adnexal mass inseparable from the ovarian tissue. It shows a classic whorled, well-circumscribed, rounded, whitish gray in color, firm and rubbery consistency. The mass was clamped, transfixed, and resected. Postoperative recovery was uneventful, and she was discharged on the third postoperative day. The specimen was sent for histopathological examination.
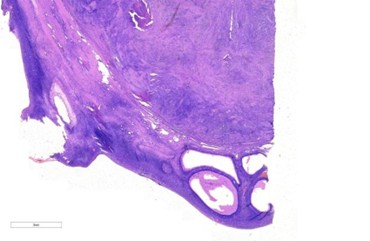
Figure 1. Resected left adnexa containing ovarian tissue with large fibroid nodules.
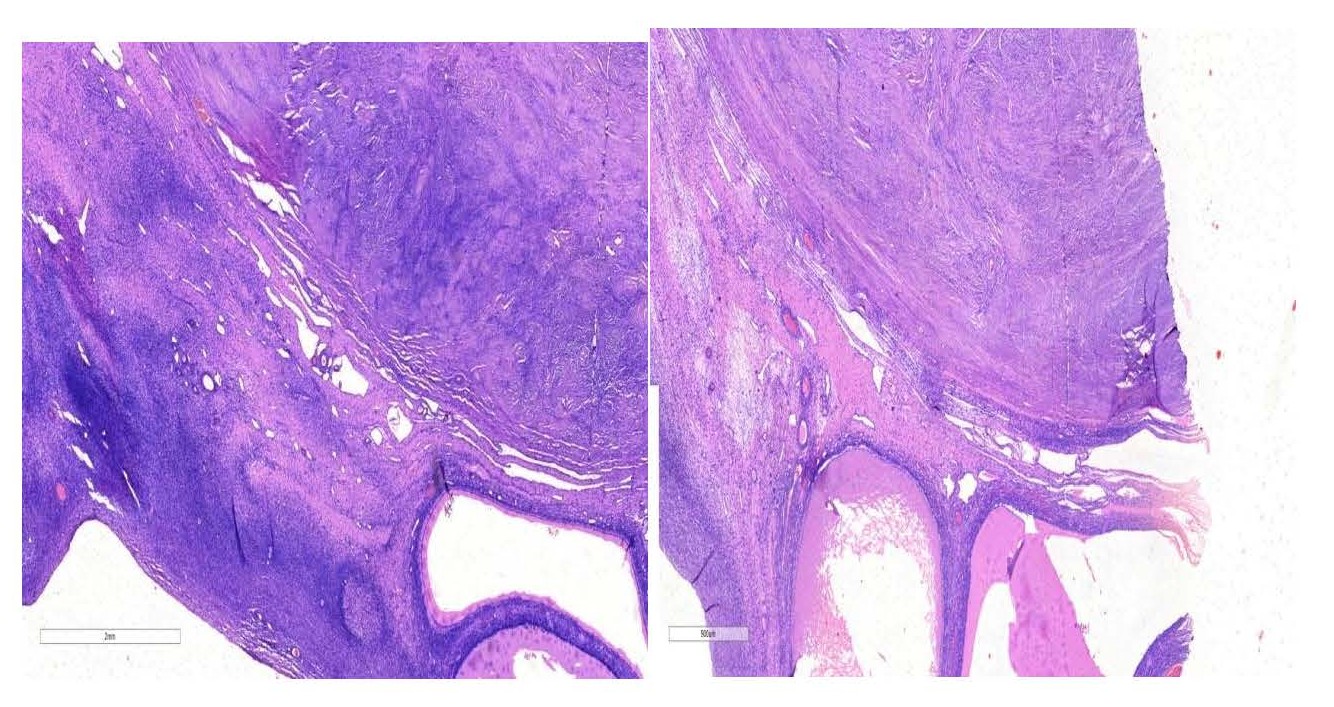
Figure 2. Micrograph demonstrating leiomyoma adjacent to ovarian tissue containing cystic follicles (×20 magnification).
Figure 3. Micrographs showing leiomyoma with adjoining ovarian tissue which shows cystic follicles X40 magnification.
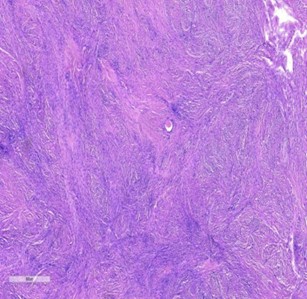
Figure 4. Micrograph showing the leiomyoma composed of interlacing fascicles of smooth muscle cells and interspersed blood vessels X40 magnification.
Discussion
The occurrence of extra-uterine leiomyomas is most commonly attributed to pedunculated subserosal fibroids that become adherent to adjacent structures such as the broad ligament, omentum, or retroperitoneum. These lesions may develop a new blood supply, undergo torsion, and lose their original uterine attachment, resulting in a parasitic leiomyoma [2,3,8]. Iatrogenic mechanisms have also been described, particularly following morcellated hysterectomies or myomectomies, where fibroid fragments detach, implant within the peritoneal cavity, and establish vascular connections from non-uterine sources such as the mesentery or bladder [6]. A similar process can occur after uterine artery embolization, with devascularized fibroid tissue detaching and reimplanting into highly vascular sites [3,9].
Clinical diagnosis of extra-uterine leiomyomas can be challenging due to their non-specific presentation and imaging features. Many cases are identified incidentally during laparotomy or confirmed histologically [3,6]. Presentations vary and may include an abdominopelvic mass, chronic abdominal pain, recurrent urinary tract infections from mass effect, small bowel obstruction, or, rarely, acute abdominal sepsis requiring bowel resection [1,7,8]. The differential diagnosis is broad and includes solid ovarian tumors, gastrointestinal stromal tumors (GISTs), bladder wall tumors, ectopic kidneys, abdominal wall lesions, lymphomas, and extra-uterine adenomyomas [6,7].
Imaging plays a key role in evaluation, although pelvic ultrasound may miss lesions in the upper abdomen. CT or abdominopelvic scans provide more information but may remain non-specific. MRI is valuable for diagnosis and surgical planning, although precise localization of the lesion can still be difficult in some cases [6,7,10]. Surgical resection, either via laparotomy or laparoscopy, remains the mainstay of treatment, with the approach determined by lesion size, location, and proximity to vital structures and presentation [7,8,10]. Alternative management strategies include expectant observation or medical therapy with gonadotropin-releasing hormone agonists, progestins, or aromatase inhibitors [7]. Our patient had presented as acute abdomen and subsequently had emergency laparotomy.
Conclusion
In conclusion, extra-uterine leiomyomas represent a rare but important clinical entity arising through diverse pathogenic mechanisms, including detachment of pedunculated subserosal fibroids, iatrogenic implantation following surgical procedures, and possibly genetic or metaplastic processes. Their diagnosis is often challenging due to nonspecific symptoms and imaging findings, necessitating a high index of suspicion and multimodal evaluation. Surgical excision remains the cornerstone of management, tailored to lesion characteristics and patient factors, while medical therapies may offer adjunctive benefit in select cases. Awareness of this condition is essential to guide appropriate diagnosis, avoid misdiagnosis, and optimize patient outcomes, particularly given the potential for significant morbidity associated with delayed or inadequate treatment.
Consent
A written informed consent was obtained from the patient for publication of this case report.
Conflicts of Interest
No conflict of interest to declare.
References
2. Nishi Gupta, Deep Shikha, Amrita Roy, Sneha Singh. Broad ligament fibroid as an incidental finding in an unruptured ectopic. Int J Clin Obstet Gynaecol 2022;6(4):05–06.
3. Amisu M, Chionuma J, Odeyemi A, Odetayo O. Prevalence and pattern of renal complications of uterine fibroids in a Teaching Hospital in Nigeria. Afr Health Sci. 2024 Dec;24(4):156–62.
4. Idowu BM, Ibitoye BO, Oyedepo VO, Onigbinde SO, Okedere TA. Ultrasonographic characterisation of obstructive uropathy in Nigerian women with uterine fibroids. Niger Postgrad Med J. 2018 Oct-Dec;25(4):220–4.
5. Wang J, Liu G, Yang Q. Parasitic myoma after transabdominal hysterectomy for fibroids: a case report. BMC Womens Health. 2023 Jun 16;23(1):310.
6. Pai AH, Yen CF, Lin SL. Parasitic Leiomyoma. Gynecol Minim Invasive Ther. 2020 Apr 28;9(2):108–9.
7. Murakami K, Kitade M, Kumakiri J, Takeuchi S, Kawasaki Y, Ochiai A, Yanagihara Y, Itakura A. Incidence and risk factors of parasitic myoma after laparoscopic myomectomy using uncontained power morcellation: Retrospective analysis of 87 patients who had a subsequent second laparoscopic surgery. J Obstet Gynaecol Res. 2024 Nov;50(11):2131–7.
8. Tunau KA, Garba JA, Panti AA, Shehu CE, Adamu AN, AbdulRahman MB, et al. Low plasma vitamin D as a predictor of uterine fibroids in a nigerian population. Niger Postgrad Med J. 2021 Jul-Sep;28(3):181–6.
9. Eyong E, Okon OA. Large Uterine Fibroids in Pregnancy with Successful Caesarean Myomectomy. Case Rep Obstet Gynecol. 2020 Nov 10;2020:8880296.
10. Igbodike E, Iwuala I, Mbonu C, Okechukwu U, Funtua A, Eleje G, et al. Giant "Hydra Headed" Uterine Fibroid in a Nullipara: A Case Report. Clin Med Insights Case Rep. 2024 Sep 10;17:11795476241274689.