Abstract
Irradiation is considered as one of the causes that may inhibit tooth development. Radiation exposure during the period of tooth development may result in impaired, delayed, or absolute failure to develop/eruption of the tooth. Radiation exposure at high dosage may also impair facial development in the pediatric population who had received radiation therapy for a malignant tumor in the head and neck region. Here we reported a case of Radiation-Induced Radicular Hypoplasia (RIRH) in a 19-year-old patient who received radiotherapy ten years ago for the Embryonal Rhabdo Myo Sarcoma of the soft palate. This case helps the clinician to observe some of the unusual and long term effects of radiotherapy on the dental structures, particularly the roots. The clinicians should consider radicular hypoplasia secondary to radiotherapy at the early stages of life if such findings are noted on the radiographs.
Keywords
Teeth Hypoplasia, Radiotherapy, Radiation Induced Radicular Hypoplasia, Dentine dysplasia, Dentinogenesis imperfecta
Introduction
Irradiation is one of the potential causes that may inhibit tooth development. Radiation may result in impaired, delayed or failure of tooth development or eruption. Also, severe consequences such as impaired facial development can be seen in the pediatric population who had received radiation therapy for malignant tumor in the head and neck region [1]. Murai T (1954) reported radiation injury to the teeth and jaws in a 12 year girl who received radiotherapy for a period of three years started at the age of 47 days for hemangioma simplex of skin of the mandible [2]. In 1973 Wilson reported a case of teeth hypoplasia in a seven year old boy who received radiotherapy for the treatment of small cell carcinoma of hard palate at the age of four months [3]. In 1994 Takinami S et al. described hypoplasia of the teeth and mandible in four year old boy who received radiation at the age of seven months for cystic hygroma of neck [4]. Hertwig’s epithelial root sheath (HERS) is important for the root formation. HERS induces the mesenchymal cells of dental papilla to develop into the odontoblast and also determine the shape and size of the root. Cementoblast and odontoblast are responsible for cementum and dentine formation of the root respectively [5]. Appropriate root size and shape supports the crown and further helps in delivering and distributing optimum masticatory forces to the bone [4]. Liest (1995) reported that odontoblast is more sensitive to radiation in comparison to ameloblast [6]. Therefore it could be hypothesized that exposure to radiation during the root development period either inhibit the development of the HERS or inhibit odontoblast resulting into the radicular agenesis or hypoplasia. The present case report discusses a rare case of radicular hypoplasia in a 19-year-old patient who was irradiated for the Embryonal Rhabdo Myo Sarcoma (ERMS) of the soft palate at the age of nine years.
Case Report
A 19-year-old female patient reported to the department for routine checkup. The patient had history of ERMS of soft palate ten years ago. She underwent wide excision of the soft palatal tumor and reconstruction with bilateral pedicled myocutaneous buccal flap ten years ago. Patient was kept under Intergroup Rhabdo Myo Sarcoma (IRMS) group IV protocol (IRS IV protocol included eight week chemotherapy alone with vincristine and from ninth week of chemotherapy patient had received local radiotherapy to the nasopharyngeal and bilateral face and neck region. Plane I: 41.4 Gray/23 fractions/32 days and Plane II: 10.8 Gray/6 fractions/8 days).
She had received Vincristine (Vincristine Sulfate 1mg by Intas Pharmceutical ltd.) for nine weeks. Indigenous radiotherapy stimulator model 2011 developed by Bhabha Atomic Research Centre, Mumbai was used as Gamma Irradiator using Co-60. The power of gamma irradiator Co-60 used was 1132 "Ci.s-1"
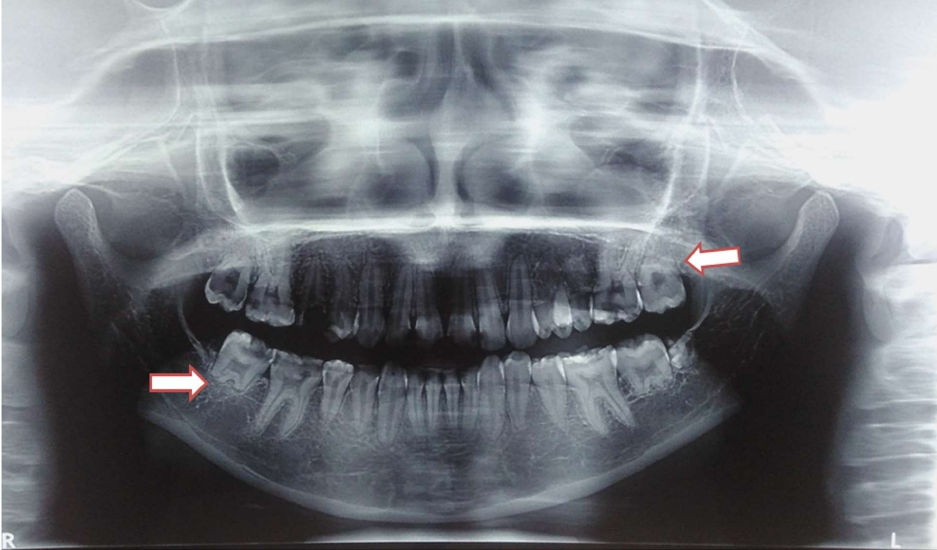
Patient received External Beam Radiation Therapy (EBRT) ten years ago. EBRT detail was 41.4 Gray/23 fractions/32 days to bilateral face and neck by bilateral portals using Cobalt 60 gamma radiation at the rate of 180 centigrays per fraction followed by a dose of 10.8 Gray/6 fractions/8 days. Total dose received by the patient was 52.2 Gray/29 fractions/40 days. A Panoramic radiograph (PAN) was advised. PAN revealed radicular hypoplasia (arrow in figure) in relation to both maxillary and mandibular second molars with missing maxillary third molars bilaterally and mandibular right third molar. Also crown of mandibular left third molar was malformed. All canines and premolars were present with stunted roots. Further, hypoplastic condyles were also seen (Figure 1). Diagnosis of Radiation Induced Radicular Hypoplasia (RIRH) was made in relation to both maxillary and mandibular second molars. Differential diagnoses of dentine dysplasia and dentinogenesis imperfecta were excluded because of their generalized nature along with peculiar features.
Figure 1: PAN showing radicular hypoplasia in relation to second molars (arrows), stunted roots of canine and premolars and condylar hypoplasia.
Discussion
Radiation causes various dental anomalies by directly affecting the developing tooth germ. As to the best of our knowledge there is scarcity in the literature on RIRH in humans. However, there are many studies that have been conducted to observe the effect of radiation on the rat jaw. Ide et al. (2014) suggested that irradiation to the head of rat causes the disturbance in the dynamics of HERS which is responsible for root formation resulting in its early disappearance in comparison to the control group [7]. In this case report, the patient had received the radiation during the probable period of root formation of the premolars and molars which later resulted in hypoplasia of the root of second molars, stunted roots of canines and premolars. Ide et al. (2014) found that there was dose dependent reduction in the proliferating cells in the periapical dental pulp and periodontal ligament surrounding HERS [7]. They suggested that using high dose [10-20 Gray (Gy)] to mouse head induced abnormal dental root structure. Lines et al. reported that radiation exposure of about 4 to 16 Gy to the tooth bud and mandibular growth centers result into the premature apical closure and radicular hypoplasia [8]. Tasaka H suggested that a dose of 24 Gray can cause interrupted tooth formation and bone development [9]. In present case patient received dose of 52.2 Gray which is much higher than the dose that causes radicular hypoplasia, interruption in the development of tooth and bone. Here we can say that the third molar tooth buds degenerated because of high dose exposure. Itoiz et al. (1983) reported formation of abnormally calcified tissue in form of osteodentine due to impaired odontoblast after irradiation of the rat incisor [10]. In this case, radiopacity in the region of mandibular left third molar can be appreciated on PAN which can be suggestive of abnormal calcified tissue in form of osteodentine, however the exact nature of tissue can be confirmed only after histological examination. We differentially diagnosed our case from dentine dysplasia type I (radicular) and dentinogenesis imperfecta. Dentine dysplasia has abnormal root and peculiar presentation of thistle tube appearance in the pulp chamber of single rooted teeth and shallow “W” in the molars’ roots. In dentinogenesis imperfecta typical presentation of bulbous crown with cervical constriction with shorter and narrow roots is seen. These findings of dentine dysplasia and dentinogenesis imperfecta were not seen in our case hence these diagnoses were excluded.
This case makes the clinician aware and adds to the evidence of some of the unusual effects of radiotherapy on the dental structures, especially to the roots. The clinicians should consider radicular hypoplasia secondary to radiotherapy if such findings are noted on the radiographs.
Conflict of Interest
Dr. Mohd Saalim, Dr. Kaustubh Sansare, Dr. Freny R. Karjodkar, Dr. Bushra Rahman, Dr. Ibrahim K Ali and Dr. Huma Parveen declare that they have no conflict of interest.
Human Rights Statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed Consent
Informed consent was obtained from patient for being included in this case report.
References
2. Murai T. Case report of radiation injury of teeth and jaws. Bull. Tokyo Med. Dent. Univ. 1954;1:71-5.
3. Wilson EH. A case showing the effect of radium therapy on developing tooth structures. Br Dent J. 1953;18:82-4.
4. Takinami S, Kaga M, Yahata H, Kure A, Oguchi H, Yasuda M. Radiation-induced hypoplasia of the teeth and mandible: A case report. Oral Surgery, Oral Medicine, Oral Pathology. 1994 Sep 1;78(3):382-4.
5. Cate AT. The role of epithelium in the development, structure and function of the tissues of tooth support. Oral Diseases. 1996 Mar;2(1):55-62.
6. Leist M. Über Röntgenschädingung der Zähne. Z Stomat. 1925;23:797-801.
7. Ide Y, Nakahara T, Nasu M, Ishikawa H. Cell dynamics in H ertwig's epithelial root sheath and surrounding mesenchyme in mice irradiated to the head. Oral Diseases. 2015 Mar;21(2):232-9.
8. Lines LG, Hazra TA, Howells R, Shipman B. Altered growth and development of lower teeth in children receiving mantle therapy. Radiology. 1979 Aug;132(2):447-9.
9. Tasaka H. Encyclopedia of Clinical Radiology. Nakayama Syoten, Tokyo. 1985;33:227-95.
10. Itoiz ME, Lafranchi HE, Cabrini RL. Ultrastructural study of osteodentin formation induced by irradiation. Journal De Biologie Buccale. 1983 Jun;11(2):109-17.