Abstract
Introduction: Impacted Laryngeal foreign bodies usually present with acute onset of choking, cough, inspiratory stridor, hoarseness, or complete aphonia and asphyxia. Children are particularly at risk due to smaller airway calibers.
Case presentation: A 4-year-old male child presented to the pediatric emergency unit of the Lagos State University Teaching Hospital with a 3 days history of accidental ingestion of a metallic foreign body. He developed a dry cough, noisy breathing, difficulty breathing, and a low-pitched voice following the incidence. Upon clinical examination, the child was stridulous with nasal flaring, intercostal and subcostal recessions. A soft tissue X-ray of the neck and chest revealed a radio opaque object in the airway at the level of C4–C6 which is the region of the larynx. A diagnosis of laryngeal foreign body was made. Videolaryngoscopy performed under inhalational anesthesia revealed a yellow metallic rectangular object, oriented sagittally and impacted at the level of the rima glottis. The foreign body was successfully removed using a grasping forceps.
Conclusion: Impacted foreign body in the larynx is a life-threatening emergency condition. A high index of suspicion is needed together with good history and investigations to make a prompt diagnosis.
Keywords
Laryngeal foreign body, Videolaryngoscopy, Tracheostomy, Bronchoscopy
Introduction
Foreign body (FB) aspiration is an uncommon but a life-threatening emergency. It occurs more commonly among children than in adults [1]. The prevalence ranges from 57% to 80% among children under five years of age [2]. Aspirated foreign bodies may lodge in the larynx, trachea or bronchi. Impaction of foreign bodies in the larynx may depend on the shape, size of the object and the phase of breathing during the aspiration [3]. They can rapidly compromise the airway, causing apnea and acute respiratory distress. The management requires rapid diagnosis and urgent intervention to prevent mortality [4,5]. Patients with impacted laryngeal foreign bodies (LFBs) usually present with acute onset of choking, cough, inspiratory stridor, hoarseness, or complete aphonia and asphyxia. Children younger than 4 years are particularly at risk because of their smaller airway calibers, frequent oral exploration and tendency to play or talk while eating or holding objects in their mouths [2,4,5]. Adults above 65 years of age may present with LFBs secondary to accidental aspiration of dental prostheses, impaired protective airway reflexes, neurological conditions and the use of psychotropic medication [6,7]. In some cases, partial obstruction may mimic asthma or croup, leading to delayed diagnosis [8].
Case Presentation
A 4-year-old male child presented to the pediatric emergency unit of the Lagos State University Teaching Hospital with a 3 day history of accidental ingestion of a metallic foreign body. His parents described the foreign body as the metallic end of a tape rule. They were unaware of the potential hazards of allowing such an object around children, and they expressed significant guilt and emotional distress. He developed a dry cough, noisy breathing, difficulty breathing, and a low-pitched voice following the incidence. There was no history of dysphagia, odynophagia, hematemesis, or hemoptysis.
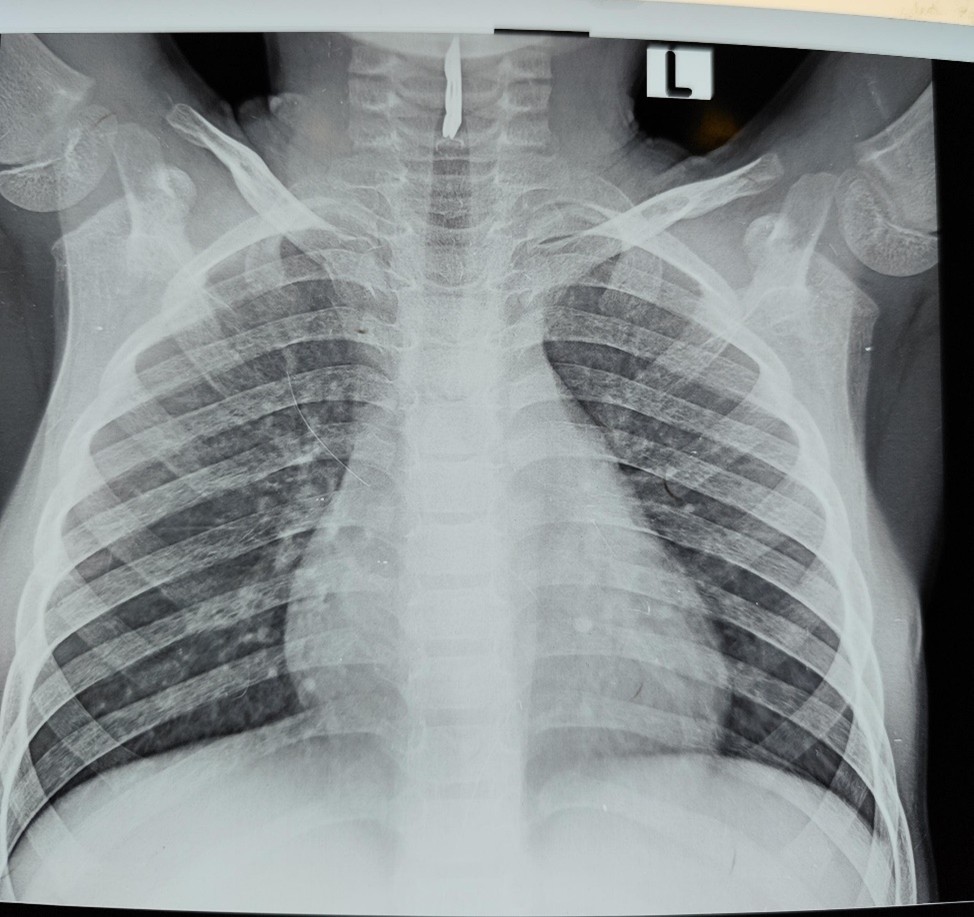
The child was stridulous on examination with nasal flaring, intercostal and subcostal recessions. He was afebrile, not pale, anicteric, not cyanosed, and not dehydrated. He was tachypneic with respiratory rate of 52 cycles/minute, oxygen saturation was 99% in room air, and other vital signs were within normal limits. A soft tissue X-ray of the neck and chest revealed a radio opaque object in the airway at the level of C4–C6 which is the region of the larynx as shown in Figures 1 and 2. A diagnosis of laryngeal foreign body was made.
Figure 1. Soft tissue X-ray of the neck and chest revealing a radio opaque object in the airway (Anterior view).
Figure 2. Soft tissue X-ray of the neck revealing a radio opaque object in the airway (Lateral view).
Figure 3. Foreign body removed from the patient.
Discussion
Impacted laryngeal foreign bodies (LFBs) are an uncommon subset of aerodigestive foreign bodies but present disproportionate risk because of their ability to acutely compromise the upper airway and precipitate life-threatening asphyxia. Children are more at risk due to their inquisitiveness, adventurous nature, lack of molars for proper mastication, playing and running with food in the mouth with consequent poor coordination in swallowing and glottic closure [9]. Also, children have smaller airway calibers and tendency to put objects in their mouths [5]. Our patient was a 4 year old boy with an appropriate neurodevelopmental milestone for age, with less risk of aspiration. This is within the age range where children are prone to aspiration which often occur accidentally [9]. Groundnuts, fish bone or whistles are the most frequently inhaled foreign bodies in this part of the world, although our patient aspirated a metallic object [9,10]. The clinical presentation of airway foreign body depends on the size, its composition, and location in the airway.
Clinical presentation is heterogeneous and ranges from dramatic acute choking and complete airway obstruction to subtle, chronic or intermittent symptoms including noisy breathing, chronic cough, dysphonia and feeding difficulties [4,5,9]. This was as the case of our patient as he developed a dry cough, noisy breathing, difficulty breathing, and a low-pitched voice following ingestion of the metallic object. The index patient aspirated a rare foreign body (the metallic end of a tape rule used for measurements, especially clothes). Also, the size was relatively large (2 cm in length by 1.5 cm in width). The circumstances of the aspiration were not clearly known by the parents. In addition, the patient presented 3 days after the inhalation. The factors for the delay in presentation to our center may be due to inability to diagnose the condition in the Primary and Secondary health institutions due shortage of Specialist Manpower in these centers. Financial difficulty may also be a factor as the condition was sudden and the parents have to pay out of pocket in the midst of financial crises in Nigeria. Reports stress that children—may present with atypical or indolent features, and that a lack of a witnessed aspiration event often contributes to diagnostic delays. Clinicians should therefore maintain a high index of suspicion when respiratory or upper-airway symptoms are unexplained or refractory to usual therapies [4,5,11]. Beyond the physical presentation, the psychological impact of an impacted laryngeal foreign body on a patient's parents can be profound, often resulting in immediate trauma and distress, and potentially leading to long-term anxiety, hypervigilance and self-blame [12].
Diagnostic evaluation must balance speed and sensitivity. Plain radiographs are widely available and are helpful when the object is radiopaque, but they may miss radiolucent items (plastic toys) and have documented false-negative rates [11]. In such cases, a high index of suspicion is required to recognize the presence of lack of complete lucency in the airway. It was estimated that only around 26% of the aspirated FBs are radio-opaque and visible on chest radiographs [13]. Management principles prioritize airway security followed by safe extraction. For definitive removal, rigid laryngoscopy under general anesthesia is the preferred approach in most series because it provides direct control of the airway, allows manipulation with specialized instruments (forceps, graspers, retrieval baskets), and permits rapid conversion to a surgical airway if extraction fails or the airway is lost [5]. In our patient, the laryngeal foreign body was successfully removed with a grasping forceps from the patient’s airway using a videolaryngoscope. No complication was observed in our patient as he was stable after the procedure. Complications and outcomes depend on timeliness of diagnosis and execution of treatment. Short-term complications include hypoxia, laryngeal mucosal laceration, bleeding, laryngospasm, distal migration of the foreign body into the tracheobronchial tree and pneumonia [4,8,11]. Effective management of impacted foreign bodies underscores the importance of interdisciplinary collaboration in achieving timely and accurate diagnosis as well as comprehensive care. Such coordinated efforts facilitate faster diagnosis, safer and more effective removal, reduced complication rate, and improved overall patient outcomes [14].
Prevention and public health measures are important, particularly in pediatric populations. Educational interventions for caregivers such as guidance on age-appropriate food preparation, adequate supervision, and avoidance of small objects are crucial both at home and creche settings where children may be exposed to these hazards. In addition, legislative measures addressing toy safety and chocking- hazard labelling have been advocated; several authors suggest that community education and early first-aid training (recognition of choking and prompt activation of emergency services) reduce morbidity. In healthcare settings, establishing local protocols for suspected airway foreign bodies and ensuring rapid access to specialist ENT and anesthesia services improve outcomes [11,15].
Conclusion
This case report draws attention that children can play with any object and aspirate them. Impacted foreign body in the larynx is a life-threatening emergency condition. A high index of suspicion is needed together with good history and investigations to make a prompt diagnosis. There is need to have more otorhinolaryngologists in the Secondary Health institutions to handle these cases.
References
2. Paladin I, Mizdrak I, Gabelica M, Golec Parčina N, Mimica I, Batinović F. Foreign Bodies in Pediatric Otorhinolaryngology: A Review. Pediatr Rep. 2024 Jun 19;16(2):504–18.
3. D'Souza JN, Valika TS, Bhushan B, Ida JB. Age based evaluation of nut aspiration risk. J Otolaryngol Head Neck Surg. 2020 Oct 9;49(1):73.
4. Sewwandi GA, Dhanawardhana DP, Etulgama SB. A typical presentation of a laryngeal foreign body in an infant. Ceylon J Otolaryngol. 2024 Feb 7;13(1):77–81.
5. Jain S, Kashikar S, Deshmukh P, Gosavi S, Kaushal A. Impacted laryngeal foreign body in a child: a diagnostic and therapeutic challenge. Ann Med Health Sci Res. 2013 Jul;3(3):464–6.
6. Fuentes ME, Soriano RG, Aragon M. Laryngeal foreign body impaction: A case series. J Laryngol Voice.2023 Jan 1;13(1):5–9.
7. Dodson H, Sharma S, Cook J. Foreign Body Airway Obstruction. [Updated 2024 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553186/.
8. Goulioumis AK, Peridis S, Koudmnakis E, Athanasopoulos I. A Foreign Body Lodged in the Glottis of a Toddler for a Prolonged Time: Anatomical Considerations and Review of the Literature. Cureus. 2023 Aug 31;15(8):e44489.
9. Nwawolo CC, Berdugo BK, Busari S, Soyika AS. Impacted foreign bodies in the larynx–Clinical aspects. Lag J Surg. 1998;1(1):14–8.
10. Ahmed AO, Shuiabu IY. Inhaled foreign bodies in a paediatric population at AKTH Kano-Nigeria. Niger Med J. 2014 Jan;55(1):77–82.
11. Chen Q, Chu H, Tao Y, Huang H, Peng L. Lessons Learned From 35 Cases of Laryngeal Foreign Bodies Undergoing Misdiagnosis in Pediatric Population. Ann Otol Rhinol Laryngol. 2017 Feb;126(2):146–51.
12. Begović I, Mihatov Štefanović I, Vrsalović R, Geber G, Kereković E, Lučev T, Baudoin T. PARENTAL AWARENESS OF THE DANGERS OF FOREIGN BODY INHALATION IN CHILDREN. Acta Clin Croat. 2022 Oct;61(Suppl 4):26–33.
13. Blanco Ramos M, Botana-Rial M, García-Fontán E, Fernández-Villar A, Gallas Torreira M. Update in the extraction of airway foreign bodies in adults. J Thorac Dis. 2016 Nov;8(11):3452–6.
14. Puvvada VS, Ramesh M, Chilaka RT, Dhanalaxmi D, Puvvada CS, Puvvada V. Retrospective Analysis of Laryngo-Tracheo-Bronchial Foreign Bodies in a Tertiary Care Setting and Insights on AI Detection Methods. Eur J Cardiovasc Med. 2024 Aug 31;14:885–9.
15. Wang HC, Chen YC, Pan HG, Li L, Teng YS. Tracheostomy-Assisted Foreign Body Removal: Insights From a Case Series and Literature Review. Ear Nose Throat J. 2023 Sep 25:1455613231201015.