Abstract
Proximal humerus fracture with simultaneous shoulder dislocation in children is a rare occurrence, with few reported cases. This systematic review of case reports aimed to document the outcomes of different treatment methods. A comprehensive literature search from 1980 to 2024 included case reports on traumatic shoulder fracture-dislocation in children. Eighteen studies were included, with a mean followup of 1.5 years. The cases comprised 7 boys and 11 girls, aged between 11 months and 16 years (median 6 years). The cases were divided into two groups based on epiphysealinvolvement. Group A had 11 cases (61%) with epiphyseal involvement, while Group B had 7 cases (38%) with metaphyseal fractures without epiphyseal involvement. Treatments included closed or open reduction, with or without internal fixation. All fractures healed in an average of 7 weeks, with full function restored in an average of 21.58 weeks. The review suggests that open reduction with K-wire fixation is optimal for Group A, whereas closed reduction with intramedullary fixation is more effective for Group B, offering satisfactory clinical and radiological results in a shorter time efficiently.
Keywords
Children, Shoulder, Fracture-dislocation, Glenohumeral, Humeral neck
Introduction
Proximal humerus fractures are rare in children, constituting less than 5% of paediatric fractures
[1]. Most of these fractures occur through the growth plate due to its relative weakness [2], with
Salter-Harris type I common in younger children and type II in adolescents; types III and IV are
uncommon [3]. Shoulder dislocations are also infrequent in children, with only 8 out of 500 cases
reported in those under 10 years of age [4]. The combination of a proximal humerus fracture and
shoulder dislocation is extremely rare, affecting less than 2% of the paediatric population [5]. The first
case was described in 1982 [6]. Proximal humeral metaphysis fracture-dislocations not involving the
growth plate are exceptionally unusual [7], often resulting from high-velocity trauma and typically
seen in children aged 5-12 years [8]. In children under 3 years with an unclear injury history, nonaccidental
injury should be suspected. Anterior dislocations are more common than posterior or
inferior ones. These injuries are challenging to treat, with few published cases on their management
[9]. We conducted a systematic review of reported cases from 1980 to 2024 to summarize existing
evidence and recommend optimal treatments for achieving favourable clinical and radiological
outcomes.
Methods
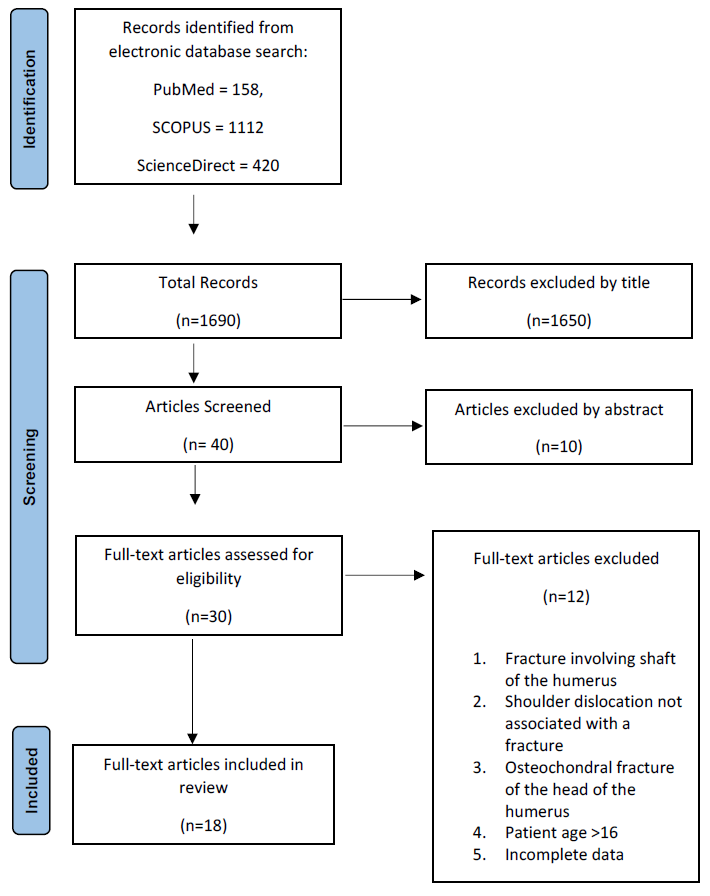
This systematic review compiles and analyses all published studies on shoulder fracture-dislocations in children. Following PRISMA guidelines, we searched databases including PubMed, Scopus, and ScienceDirect as outlined in Figure 1. Articles on traumatic shoulder fracture-dislocation in children were evaluated, and key data were extracted based on predefined criteria, including patient age, sex, diagnosis, treatment method, and clinical and radiological outcomes.
Authors’s comments on the search method We include a limited number of databases due to the following reasons. While we are open to all databases, we primarily focused on Scopus, PubMed, and ScienceDirect because they are subscribed to by our institution and readily available to us. These databases are renowned for their comprehensive and high-quality data on the specific type of fracture we were studying. Given the rarity of this fracture, we prioritized obtaining reliable and relevant data, which sometimes meant emphasizing quality over quantity. Expanding the number of databases could have introduced variability and potential inconsistencies, potentially detracting from the clarity and focus of
our analysis. For example, a search on Google Scholar returned 9,890 articles, most of which were irrelevant. Using Scopus, PubMed, and ScienceDirect, we aimed to ensure that our review was based on the most pertinent and trustworthy sources.
Figure 1: PRISMA flowchart for selection of articles in the systematic review.
Results
The search and selection process are described in Table 1, resulting in 18 studies as outlined in Table 2 after applying the following inclusion criteria.
|
PubMed |
|||
|
No |
Keywords |
Number of articles |
Search fields |
|
1 |
((fracture-dislocation) AND humeral neck) AND children |
26 |
(("fracture dislocation"[MeSH Terms] OR ("fracture"[All Fields] AND "dislocation"[All Fields]) OR "fracture dislocation"[All Fields]) AND (("humerus"[MeSH Terms] OR "humerus"[All Fields] OR "humeral"[All Fields]) AND ("neck"[MeSH Terms] OR "neck"[All Fields]))) AND ("child"[MeSH Terms] OR "child"[All Fields] OR "children"[All Fields]) |
|
2 |
fracture-dislocation AND shoulder AND Children |
103 |
("fracture dislocation"[MeSH Terms] OR ("fracture"[All Fields] AND "dislocation"[All Fields]) OR "fracture dislocation"[All Fields]) AND ("shoulder"[MeSH Terms] OR "shoulder"[All Fields]) AND ("child"[MeSH Terms] OR "child"[All Fields] OR "children"[All Fields]) AND hasabstract[text] |
|
3 |
Traumatic AND Fracture-Dislocation AND Shoulder AND Children
|
29 |
: (((Traumatic) AND ("Fracture-Dislocation")) AND (Shoulder)) AND (Children) ("traumatic"[All Fields] OR "traumatically"[All Fields] OR "traumatism"[All Fields] OR "traumatisms"[All Fields] OR "traumatization"[All Fields] OR "traumatizations"[All Fields] OR "traumatize"[All Fields] OR "traumatized"[All Fields] OR "traumatizes"[All Fields] OR "traumatizing"[All Fields]) AND "Fracture-Dislocation"[All Fields] AND ("shoulder"[MeSH Terms] OR "shoulder"[All Fields] OR "shoulders"[All Fields] OR "shoulder s"[All Fields]) AND ("child"[MeSH Terms] OR "child"[All Fields] OR "children"[All Fields] OR "child s"[All Fields] OR "children s"[All Fields] OR "childrens"[All Fields] OR "childs"[All Fields])
|
|
SCOPUS |
|||
|
1 |
fracture-dislocation AND shoulder AND Children |
103 |
("fracture dislocation"[MeSH Terms] OR ("fracture"[All Fields] AND "dislocation"[All Fields]) OR "fracture dislocation"[All Fields]) AND ("shoulder"[MeSH Terms] OR "shoulder"[All Fields]) AND ("child"[MeSH Terms] OR "child"[All Fields] OR "children"[All Fields]) AND hasabstract[text] |
|
2 |
Fracture-dislocation AND humeral neck AND children |
954 |
(("fracture dislocation"[MeSH Terms] OR ("fracture"[All Fields] AND "dislocation"[All Fields]) OR "fracture dislocation"[All Fields]) AND (("humerus"[MeSH Terms] OR "humerus"[All Fields] OR "humeral"[All Fields]) AND ("neck"[MeSH Terms] OR "neck"[All Fields]))) AND ("child"[MeSH Terms] OR "child"[All Fields] OR "children"[All Fields]) |
|
3 |
Traumatic AND Fracture-Dislocation AND Shoulder AND Children
|
55 |
(((Traumatic) AND ("Fracture-Dislocation")) AND (Shoulder)) AND (Children) ("traumatic"[All Fields] OR "traumatically"[All Fields] OR "traumatism"[All Fields] OR "traumatisms"[All Fields] OR "traumatization"[All Fields] OR "traumatizations"[All Fields] OR "traumatize"[All Fields] OR "traumatized"[All Fields] OR "traumatizes"[All Fields] OR "traumatizing"[All Fields]) AND "Fracture-Dislocation"[All Fields] AND ("shoulder"[MeSH Terms] OR "shoulder"[All Fields] OR "shoulders"[All Fields] OR "shoulder s"[All Fields]) AND ("child"[MeSH Terms] OR "child"[All Fields] OR "children"[All Fields] OR "child s"[All Fields] OR "children s"[All Fields] OR "childrens"[All Fields] OR "childs"[All Fields])
|
|
ScienceDirect |
|||
|
1 |
((fracture-dislocation) AND humeral neck) AND children |
154 |
(("fracture dislocation"[MeSH Terms] OR ("fracture"[All Fields] AND "dislocation"[All Fields]) OR "fracture dislocation"[All Fields]) AND (("humerus"[MeSH Terms] OR "humerus"[All Fields] OR "humeral"[All Fields]) AND ("neck"[MeSH Terms] OR "neck"[All Fields]))) AND ("child"[MeSH Terms] OR "child"[All Fields] OR "children"[All Fields]) |
|
2 |
Traumatic AND Fracture-Dislocation AND Shoulder AND Children
|
42 |
(((Traumatic) AND ("Fracture-Dislocation")) AND (Shoulder)) AND (Children) ("traumatic"[All Fields] OR "traumatically"[All Fields] OR "traumatism"[All Fields] OR "traumatisms"[All Fields] OR "traumatization"[All Fields] OR "traumatizations"[All Fields] OR "traumatize"[All Fields] OR "traumatized"[All Fields] OR "traumatizes"[All Fields] OR "traumatizing"[All Fields]) AND "Fracture-Dislocation"[All Fields] AND ("shoulder"[MeSH Terms] OR "shoulder"[All Fields] OR "shoulders"[All Fields] OR "shoulder s"[All Fields]) AND ("child"[MeSH Terms] OR "child"[All Fields] OR "children"[All Fields] OR "child s"[All Fields] OR "children s"[All Fields] OR "childrens"[All Fields] OR "childs"[All Fields])
|
|
|
Fracture-Dislocation AND shoulder AND Children |
224 |
("fracture dislocation"[MeSH Terms] OR ("fracture"[All Fields] AND "dislocation"[All Fields]) OR "fracture dislocation"[All Fields]) AND ("shoulder"[MeSH Terms] OR "shoulder"[All Fields]) AND ("child"[MeSH Terms] OR "child"[All Fields] OR "children"[All Fields]) AND hasabstract[text |
|
|
TOTAL |
1690 |
|
|
No |
Year |
Author |
Country |
Age |
Sex |
Mode of Injury |
Side |
Associated injury with dislocation |
Surgical treatment |
Fixation by wires/pins/ screws |
Radiological union achieved in 6 weeks |
Full movement Achieved in 12 weeks |
Final Follow-up (months) |
|
1 |
1982 |
Nicastro & Adair [6] |
USA |
32 M |
F |
NAI |
L |
Epiphysis separation (SH 1) |
Open Reduction |
Yes |
Yes |
Yes |
24 |
|
2 |
1992 |
Gregg-Smith & White [17] |
UK |
12 Y |
F |
Fall from height |
R |
Fracture epiphysis (SH 3) |
Open Reduction |
Yes |
Yes |
Yes |
4 |
|
3 |
1994 |
Obremskey & Routt [15] |
USA |
12 Y |
F |
Fall from height |
R |
Fracture Metaphysis with ep displacement (SH 2) |
Closed Reduction |
No |
Yes |
No |
8 |
|
4 |
1997 |
Wang et al. [18] |
USA |
10 Y |
M |
Fell off bicycle |
L |
Fracture epiphysis (SH 3) |
Open Reduction |
Yes |
No |
No |
24 |
|
5 |
2003 |
Winmoon et al. [11] |
Thailand |
24 M |
M |
Fall from the stroller |
L |
Epiphysis separation (SH 1) |
Closed Reduction |
Yes |
Yes |
Yes |
30 |
|
6 |
2004 |
Do & Kellar [20] |
USA |
14 Y |
F |
MVA |
R |
Fracture metaphysis with no epiphyseal involvement |
Closed Reduction |
Yes |
Yes |
No |
10 |
|
7 |
2007 |
Lee et al. [19] |
South Korea |
16 Y |
M |
Fell off bicycle |
R |
Fracture epiphysis (SH 3) |
Open Reduction |
Yes |
No |
No |
16 |
|
8 |
2010 |
Nugpok et al. [12] |
India |
36 M |
F |
Fall from height |
L |
Epiphysis separation (SH 1) |
Open Reduction |
Yes |
Yes |
Yes |
12 |
|
9 |
2013 |
Gupta et al. [13] |
India |
36 M |
M |
MVA |
L |
Epiphysis separation (SH 1) |
Closed Reduction |
Yes |
Yes |
No |
12 |
|
10 |
2013 |
Azevedo et al. [7] |
Portugal |
6 Y |
M |
Fall from height |
R |
Fracture Metaphysis with no epiphyseal involvement |
Open Reduction |
Yes |
Yes |
No |
60
|
|
11 |
2013 |
Isik et al. [8] |
Turkey |
7 Y |
F |
Fall from height |
L |
Fracture Metaphysis with ep displacement (SH 2) |
Open Reduction |
Yes |
Yes |
Yes |
6 |
|
12 |
2014 |
Jonghun et al. [9] |
South Korea |
5 Y |
F |
Fall from height |
R |
Fracture Metaphysis with no epiphyseal involvement |
Open Reduction |
Yes |
No |
Yes |
12 |
|
13 |
2015 |
Hong et al. [16] |
South Korea |
9 Y |
M |
Fall from height |
L |
Fracture Metaphysis with ep displacement (SH2) |
Open Reduction |
Yes |
Yes |
No |
12 |
|
14 |
2017 |
Jin et al. [10] |
China |
6 Y |
F |
Fall from height |
R |
Fracture Metaphysis with no epiphyseal involvement |
Open Reduction |
Yes |
Yes |
No |
24 |
|
15 |
2017 |
Fannouch et al. [21] |
Saudi Arabia |
10 Y |
M |
Fell off stairs |
L |
Fracture Metaphysis with no epiphyseal involvement |
Closed Reduction |
Yes |
Yes |
Yes |
4 |
|
16 |
2020 |
Ikram et al. [22] |
Malaysia |
6 Y |
F |
MVA |
R |
Fracture Metaphysis with no epiphyseal involvement |
Closed Reduction |
Yes |
Yes |
Yes |
12 |
|
17 |
2021 |
Young & Mantica [14] |
USA |
11 M |
M |
NAI |
R |
Epiphysis separation (SH 1) |
Open Reduction |
No |
Yes |
No |
24 |
|
18 |
2021 |
Al-Omari et al. [23] |
Jordan |
5 Y |
F |
Fall from height |
L |
Fracture Metaphysis with no epiphyseal involvement |
Open Reduction |
Yes |
Yes |
No |
36 |
Inclusion criteria
The inclusion criteria involved all case reports from 1980-2024 of children who underwent closed or open reduction for traumatic fracture-dislocation of the shoulder, with no exclusions based on geography or language. We included only cases with imaging evidence of a fracture involving the epiphysis or metaphysis of the humerus, accompanied by a shoulder joint dislocation following a traumatic episode.
In recent years, there have been reported cases in the literature that were not included due to our strict inclusion criteria. For instance, in 2022, Fettah et al. [24]. reported a fracture-dislocation of the left shoulder in a 14-year-old girl from group A. The treatment was successfully performed using a combination of closed intramedullary K-wire fixation for the fracture and open reduction for the dislocation. However, the follow-up data was missing, so we did not include it in our review.
In 2024, Navaeifar et al. [25]. reported a case of anterior dislocation in a 6-year-old child with a fracture. Since the fracture involved the clavicle, it was not considered in our review.
The patient cohort consisted of 10 girls and 8 boys, with a median age of 6 years. The most common injury mechanisms were falls from height (9 cases) and road traffic accidents (3 cases). The cases were categorized into two groups based on epiphyseal involvement as shown in Tables 3 and 4.
- Group A (with epiphyseal involvement): 11 cases (61%), comprising 6 boys and 5 girls, with 7 left-sided and 4 right-sided injuries. Of these, 8 (72%) were anterior dislocations, 2 (18%) were posterior, and 1 was (9%) inferior.
- Group B (without epiphyseal involvement): 7 cases (39%), comprising 5 girls and 2 boys, with 5 right-sided and 2 left-sided injuries. Six (85%) were anterior dislocations and 1 (15%) was posterior. The median age in this group was 6 years.
|
No |
Author |
Age (Years) |
Traumatic event |
Type of Dislocation |
Type of SH Injury |
Surgical Approach |
Method of fixation |
Immobilize (weeks) |
Radiological Union (weeks) |
Full move (weeks) |
Final Follow up(years) |
Outcome |
|
1 |
Nicastro & Adair [6] |
2.6 |
Fall from the crib, NAI |
Anterior |
Type I |
Open reduction |
One K-wire |
3 |
3 |
7 |
2 |
Uneventful |
|
2 |
Winmoon et al. [11] |
2 |
Fall from the stroller |
Anterior |
Type I |
Closed reduction |
Two K-wires |
3 |
6 |
12 |
2.5 |
uneventful |
|
3 |
Nugpok et al. [12] |
3 |
Fall from a height while playing |
Anterior |
Type I |
Open reduction |
Two K-wires |
4 |
6 |
12 |
1 |
Uneventful |
|
4 |
Gupta et al. [13] |
3 |
Road traffic accident |
Anterior |
Type I |
Closed reduction |
Three K-wires |
6 |
8 |
8 |
1 |
Uneventful |
|
5 |
Young & Mantica [14] |
0.9 |
Arm stuck in the crib, NAI |
Anterior |
Type I |
Open with no fixation |
Body-bandage |
2 |
6 |
24 |
2 |
uneventful |
|
6 |
Obremskey & Routt [15] |
12 |
Fell off height, 22 m |
Anterior |
Type II |
Closed reduction |
Sling |
6 |
6 |
76 |
1.2 |
Axillary N -resolved in 6 weeks |
|
7 |
Isik et al. [8] |
7 |
Fell 1.5m height |
Inferior |
Type II |
Open reduction |
Two K-wires |
4 |
6 |
12 |
0.5 |
uneventful |
|
8 |
Hong et al. [16] |
9 |
Fell 1 m height |
Posterior |
Type II |
Open reduction |
Four K-wires |
4 |
6 |
24 |
1 |
Uneventful |
|
9 |
Gregg-Smith & White [17] |
12 |
Fell off horse |
Anterior |
Type III |
Open reduction |
One K-wire |
3 |
4 |
6 |
0.3 |
Uneventful |
|
10 |
Wang et al. [18] |
10 |
Fell off bicycle |
Anterior |
Type III |
Open reduction |
Two lag screws |
6 |
6 |
52 |
2 |
AVN but revascularized |
|
11 |
Lee et al. [19] |
16 |
Fell off bicycle |
Posterior |
Type III |
Open reduction |
Three Steinmann pins |
4 |
8 |
52 |
1.5 |
Localized avascular necrosis of the humeral head. |
|
No |
Author |
Age (years) |
Traumatic event |
Type of Dislocation |
Associated Injury |
Surgical Approach |
Method of fixation |
Immobilize (weeks) |
Radiological Union (weeks) |
Full movement (weeks) |
Final follow up (years) |
Outcome |
|
1 |
Do & Kellar [20] |
14 |
MVA |
Inferior |
Fracture metaphysis with no epiphyseal involvement |
Closed
|
Four K-wires |
6 |
6 |
24 |
1 |
Uneventful |
|
2 |
Azevedo et al. [7] |
6 |
Fell off tractor |
Anterior |
Fracture metaphysis with no epiphyseal involvement |
Open |
Two K-wires |
4 |
8 |
30 |
5 |
Uneventful
|
|
3 |
Jonghun et al. [9] |
5 |
Fell off tree |
Inferior |
Fracture metaphysis with no epiphyseal involvement |
Open |
4 K-wires |
6 |
12 |
12 |
1 |
uneventful |
|
4 |
Jin et al. [10]
|
6 |
Fell off a ladder |
Anterior |
Fracture metaphysis with no epiphyseal involvement |
Open |
Two ESIN |
4 |
8 |
36 |
2 |
Uneventful |
|
5 |
Fannouch et al. [21] |
10 |
Fell off stairs |
Posterior |
Fracture metaphysis with no epiphyseal involvement |
Closed |
Two TENS/intra-medullary |
4 |
8 |
8 |
4 |
Uneventful |
|
6 |
Ikram et al. [22] |
6 |
MVA |
Anterior |
Fracture metaphysis with no epiphyseal involvement |
Closed |
Two K-wires/intra-medullary |
4 |
6 |
12 |
24 |
Uneventful |
|
7 |
Al-Omari et al. [24] |
5 |
Fell off 2m |
Anterior |
Fracture metaphysis with no epiphyseal involvement |
Open |
Three K-wires |
4 |
8 |
24 |
3 |
Uneventful |
Treatment
In Group A, three children with SH type I injuries underwent open reduction and two underwent closed reduction, all with K-wire fixation. Those treated with closed reduction regained full movement in 6 weeks, earlier than those with open reduction. For SH type II, two children had open reduction and one had closed reduction with K-wire fixation. All three children with SH type III injuries were treated with open reduction and K-wire fixation.
In Group B, four cases had open reduction with K-wire or elastic stable intramedullary nail (ESIN) fixation, while three cases had closed reduction with intramedullary and percutaneous fixation, performed through a posterolateral approach at the distal humerus. All intramedullary devices passed through the epiphysis, and no cases of early epiphyseal closure or avascular necrosis (AVN) were reported.
Discussion
Trauma to the shoulder can cause various injuries, including rotator cuff strain, glenohumeral subluxation, proximal humerus fractures, and joint dislocations. Paediatric proximal humerus fractures are rare, accounting for 2% of paediatric fractures and 3-6.7% of physeal fractures [1,3]. Combined fractures and shoulder dislocations in children are extremely rare, typically resulting from high-energy trauma. Over the past 40 years, only 18 cases have been reported, with an increase over the last 10 years [26]. This trend is illustrated in Figure 2.
Figure 2: Trends in Publications of Case Reports from 1980-2024.
When the injury history is vague, non-accidental injury (NAI) should be suspected. A thorough examination and skeletal surveys are recommended to rule out NAI, as seen in two reported cases [6,14].
Proximal humerus fractures in children can be categorized based on growth plate involvement. Younger children typically sustain Salter-Harris (SH) type I fractures, while older children (5-12 years) often have metaphyseal fractures without physis involvement.
Five cases of SH type I injuries, all involving anterior dislocation, have been reported. Two cases were suspected of non-accidental injury (NAI). Closed reduction succeeded in two children due to a partially intact periosteum and capsule, while the other three required open reduction [13]. The closed reduction cases achieved full movement more quickly.
Three cases of SH type II injuries occurred in older children. One case, managed with closed reduction, took 8 months for fracture remodelling and 76 weeks for full recovery. The other two, treated with open reduction and K-wire fixation, recovered fully in 12 and 24 weeks [15].
SH type III injuries are rare, occurring in adolescents and requiring open reduction due to complex fracture patterns. The incidence of avascular necrosis (AVN) is high (66.6%) but was not seen when smooth K-wires were used [18].
In Group B, seven cases were involved shoulder dislocation with metaphyseal fractures but no epiphysis involvement. Non-operative treatment is generally recommended due to children's high remodelling capacity. However, for combined dislocations and fractures, most authors recommend reduction and internal fixation to prevent complications [5]. Successful closed reduction and intramedullary fixation were achieved in some cases [21,22], while others required open reduction [7,9,10,23]. There was no significant difference in radiological union and functional recovery between closed and open reductions for these injuries.
Conclusion
For injuries affecting the epiphysis, open reduction with pin fixation is recommended to achieve an anatomical position of the epiphyses and humeral head. In cases without epiphyseal injury, closed reduction with intramedullary fixation allows for a quicker return to full shoulder movement compared to open reduction. Proper pre-operative imaging is essential to accurately assess the humeral head position before surgery to ensure normal anatomical restoration.
Limitations
One of the primary limitations of our mini- review is using only three databases: PubMed, Scopus, and ScienceDirect. This selective approach might have restricted the comprehensiveness of our review by potentially excluding relevant studies that are indexed in other databases.
By not including additional databases such as Embase, Cochrane Library, or Web of Science, we may have missed pertinent research, leading to potential publication bias.
Our choice was influenced by the availability of subscriptions and the known reliability and relevance of these databases to our specific research topic. While these databases provided high-quality and comprehensive data on the rare fracture type we studied, future reviews could benefit from a broader database search to ensure an even more exhaustive collection of relevant literature. This broader approach could help mitigate the risk of missing valuable studies and provide a more balanced and comprehensive understanding of the topic.
References
2. Sanders JO. Fractures and dislocations of the humeral shaft and shoulder. Fractures in Children. 1996:905-1019.
3. CHARLES S NEER II, HoRwITz BS. Fractures of the proximal humeral epiphysial plate. Clinical Orthopaedics and Related Research®. 1965 Jul 1;41:24-31.
4. Rowe CR. Prognosis in dislocations of the shoulder. JBJS. 1956 Oct 1;38(5):957-77.
5. Bishop JY, Flatow EL. Pediatric shoulder trauma. Clinical Orthopaedics and Related Research (1976-2007). 2005 Mar 1;432:41-8.
6. Nicastro JF, Adair DM. Fracture-dislocation of the shoulder in a 32-month-old child. Journal of Pediatric Orthopaedics. 1982 Oct 1;2(4):427-9.
7. Azevedo J, Maia B, Correia J. Fracture-dislocation of the proximal humerus in a 6-year-old child: case report. Journal of Shoulder and Elbow Surgery. 2013 Jun 1;22(6):e16-9.
8. Isik M, Subasi M, Cebesoy O, Koca I, Pamukcu U. Traumatic shoulder fracture-dislocation in a 7-year-old child: a case report. Journal of Medical Case Reports. 2013 Jun 20:7:156.
9. Ji J, Mohamed S, Sang-Eun P, Po YP. A severely displaced metaphyseal fracture of the proximal humerus with dislocation of the shoulder in a child. Chinese Journal of Traumatology. 2014 Feb 1;17(01):54-6.
10. Jin S, Cai H, Xu Y. Shoulder dislocation combined with proximal humerus fracture in children: a case report and literature review. Medicine. 2017 Dec 1;96(48):e8977.
11. Winmoon C, Sathira-Angkura V, Kunakornsawat S, Prasartritha T. Fracture-dislocation of the glenohumeral joint in a 2-year-old child: case report. Journal of Trauma and Acute Care Surgery. 2003 Feb 1;54(2):372-5
12. Nugpok O, Menon J, Satyanarayana P. Fracture dislocation shoulder in a 3-year old. European Journal of Orthopaedic Surgery & Traumatology. 2010 May;20:333-4.
13. Gupta R, Singh A, Singh KK, Vohra R. Fracture of proximal humerus with dislocation of glenohumeral joint in a 3 year old child: a case report. Journal of Orthopaedic Case Reports. 2013 Jan-Mar;3(1):26-8.
14. Young JR, Mantica AL. Open reduction of a fracture-dislocation of the shoulder in an 11-month-old child: a case report. JBJS Case Connector. April-June 2021; 11 (2): e20.01037.
15. Obremskey W, Routt MC. Fracture-dislocation of the shoulder in a child: case report. Journal of Trauma and Acute Care Surgery. 1994 Jan 1;36(1):137-40.
16. Hong S, Nho JH, Lee CJ, Kim JB, Kim B, Choi HS. Posterior shoulder dislocation with ipsilateral proximal humerus type 2 physeal fracture: case report. Journal of Pediatric Orthopaedics B. 2015 May 1;24(3):215-8.
17. Gregg-Smith SJ, White SH. Salter-Harris III fracture-dislocation of the proximal humeral epiphysis. Injury. 1992;23(3):199-200.
18. Wang P, Koval KJ, Lehman W, Strongwater A, Grant A, Zuckerman JD. Salter-Harris type III fracture-dislocation of the proximal humerus. Journal of Pediatric Orthopaedics B. 1997 Jul 1;6(3):219-22.
19. Lee SH, Lee DH, Baek JR. Proximal humerus Salter type III physeal injury with posterior dislocation. Archives of Orthopaedic and Trauma Surgery. 2007 Feb;127:143-6.
20. Do T, Kellar K. Transitory inferior dislocation of the shoulder in a child after shoulder injury: a case report and treatment results. The Iowa Orthopaedic Journal. 2004:24:119-22.
21. Fannouch G, Al Khalife YI, Al Turki AS, Jawadi AH. Traumatic pediatric shoulder fracture dislocation treated with closed reduction and intramedullary nailing: A case report. Trauma Case Reports. 2017 Jun 4:9:22-26.
22. Ikram MA, Premdas VB, Alias MS. Traumatic shoulder fracture-dislocation in a child: An innovative method of closed reduction. Trauma. 2021 Jan;23(1):64-9.
23. Al-Omari AA, Alrawashdeh M, Obeidat O, Al-Rusan M, Essa SB, Radaideh AM, et al. Entrapped long head of biceps tendon in pediatric proximal humerus fracture dislocation: a case report and review of the literature. Annals of Medicine and Surgery. 2021 Jun 23:67:102510.
24. Fettah M, Oualili I, Mimouni M, Jabri H, Abdellaoui H, Atarraf K, et al. Traumatic pediatric shoulder fracture-dislocation in a 14-year-old child. Journal of Pediatric Surgery Case Reports. 2022 Apr 1;79:102202.
25. Navaeifar N, Afshar A, Tabrizi A, Shariyate MJ. Anterior Shoulder Dislocation and Clavicle Fracture in a 6-year-old Boy: A Case Report and Literature Review. JSES Reviews, Reports & Techniques. 2024 Feb 21;4(2):312-314.
26. Ikram MA, Burud I, Akbar Z, Fadhlina Binti Hisham S. Management of traumatic fracture–dislocation of the shoulder in children: A systematic review of published case reports. Trauma. 2024 Apr;26(2):101-12.