Abstract
Background: Silver Trauma refers to the specialized approach in managing trauma in patients over the age of 65. The use of Silver Trauma frameworks can have positive outcomes across all measurable domains in healthcare. Our paper aimed to assess factors that positively and negatively influence length of stay (LOS), functional outcomes on discharge as evidenced by discharge destination (DD), and readmission rates.
Materials and Methods: A retrospective analysis was conducted over a 3-month period in a District General Hospital. We assessed for factors that positively and negatively influenced LOS, DD, and readmission rates. In particular, the factors we focused on assessing included mechanism of injury, Body Mass Index (BMI), and nutritional status as assessed by the Malnutrition Universal Screening Tool (MUST).
Results: Patients with multisystem injuries demonstrated the worst outcomes across all domains, with the longest LOS in comparison to head injury patients who had the shortest. When assessing DD, patients with multisystem injuries and thoracic injuries had the greatest reduction in functional outcomes, whilst head trauma patients had the most preserved. Malnourished patients (MUST score of 3 or above) and those with a BMI <18.5 had the least favorable outcomes in terms of LOS and DD. Interestingly, patients with a higher BMI had a reduced LOS and better functional status outcomes. We found no correlation in readmission rates.
Conclusion: Our paper highlights the importance of an individualized approach in managing Silver Trauma patients. It emphasizes the importance of tertiary centers in the management of patients with multisystem injuries. Our results show that malnourished patients and those with a BMI <18.5 have poorer outcomes across most domains. The mechanism of injury also appears to influence outcomes with multisystem and thoracic injuries having poorer prognostic outcomes compared to others. This represents an area for further work.
Keywords
Laparoscopy, Proximal gastrectomy, Single muscle flap, Stomach tumors, Gastroesophageal reflux
Highlights
- Silver Trauma refers to the specialized approach in managing trauma in patients over the age of 65
- Silver Trauma frameworks have positive outcomes across all measurable domains in healthcare
- Patients with multisystem injuries demonstrated the worst outcomes across all domains
- Patients with multisystem injuries and thoracic injuries had the greatest reduction in functional outcomes, whilst head trauma patients had the most preserved
- Malnourished patients (MUST score of 3 or above) and those with a BMI <18.5 had the least favorable outcomes in terms of LOS and DD
- Patients with a higher BMI had a reduced LOS and better functional status outcomes
Introduction
Trauma is a worldwide public health concern [1]. Major trauma describes a serious injury often involving multiple organs. In the UK, the most common cause is a fall from less than 2 metres’ height, followed by road traffic accidents [2]. There are approximately 20,000 cases of major trauma each year in England and a further 28,000 cases which require a similar level of care but would not be classed as major trauma [3]. ‘Silver Trauma’ is a newer term which refers to the specialized approach for managing trauma in those over the age of 65 years, focusing on their unique needs, timely care, and appropriate management. At the cornerstone of Silver Trauma is recognition that these patients often present with different injury patterns, such as falls, and have altered physiological responses and reserves in comparison to younger patients [4]. Key components of Silver Trauma include: 1) Early Identification – recognition of elderly patients with poor physiological reserve, who require prompt and comprehensive attention [5]. 2) Multidisciplinary Approach – involvement of various specialties, such as physiotherapists, pharmacists, occupational therapists, dieticians, and care of the elderly teams, to facilitate recovery. 3) Altered management – reduced physiological reserve and medical comorbidities alter both management and recovery [5], and 4) Outcomes – Silver Trauma aims to improve measures such as quality of life (QOL) on discharge, discharge destination, and functional outcomes [6]. Although not a new concept, there remains much to be done in both promoting and implementing Silver Trauma management within hospitals. The use of a Silver Trauma framework can have positive outcomes on length of stay, not only reducing morbidity and mortality [7], but, crucially, facilitating improvements in QOL, functional outcomes on discharge, and discharge destinations (i.e. returning to the same level of care prior to admission).
We reviewed outcomes of Silver Trauma patients over a 3-month period in a busy District General Hospital. We assessed various parameters during their inpatient admission to help identify factors that help improve: length of stay (LOS), functional outcome on discharge inferred from discharge destination (DD), and readmission rates.
Methods
Data were collected retrospectively over a 3-month period between September 2024 – November 2024. All patients over the age of 65 presenting with trauma were included. Patients transferred to tertiary centers on arrival or during admission were excluded. Data collected directly from patients’ electronic records included: age, gender, initial diagnosis, number of rib fractures, presence of flail segment, non-rib fractures, presence and type of intracranial bleed, other injuries, length of stay, fall as mechanism of injury, significant renal, cardiac, or respiratory history, concomitant use of: antihypertensives, anticoagulants, or antiplatelets, comorbid diabetes, weight, BMI, MUST score, time taken to calculate MUST score, discharge destination, pre-admission residence, mortality, re-admission within 30 days, input from dietetic team, nutritional support, venous thromboembolism risk assessment.
Patients were categorized into four broad groups based on the mechanism of injuries: thoracic injuries, abdominal/pelvic (AP) injuries, head injuries, and multisystem injuries (i.e. ≥2 injuries).
Data are presented as median (range) or mean (SD) unless otherwise stated and were analyzed for: length of stay, discharge destination, and readmission rates.
Results
Patient demographics
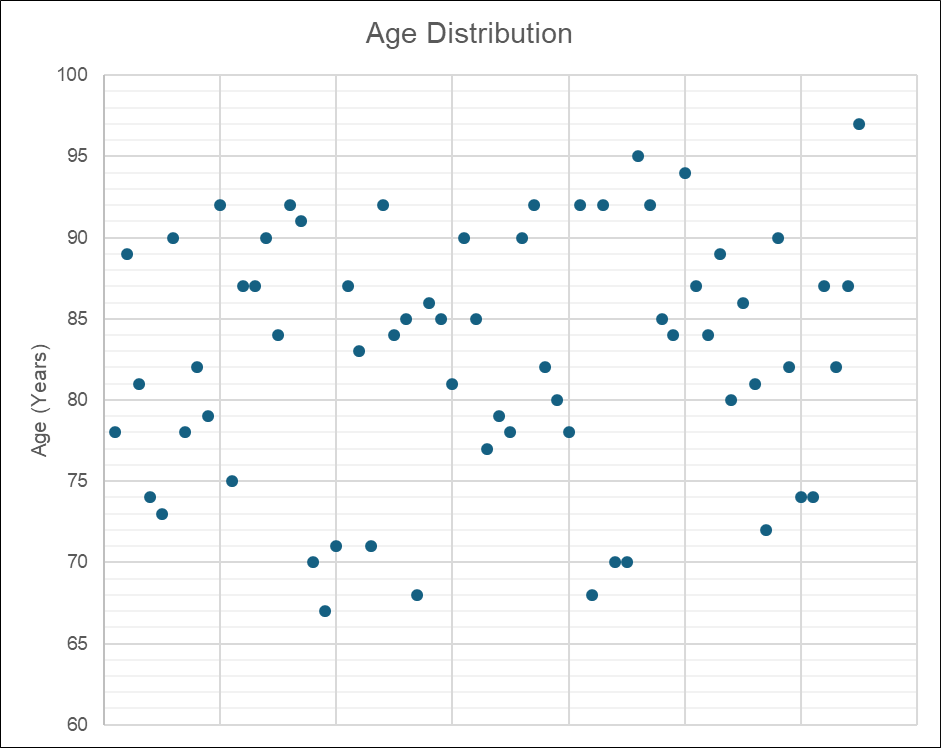
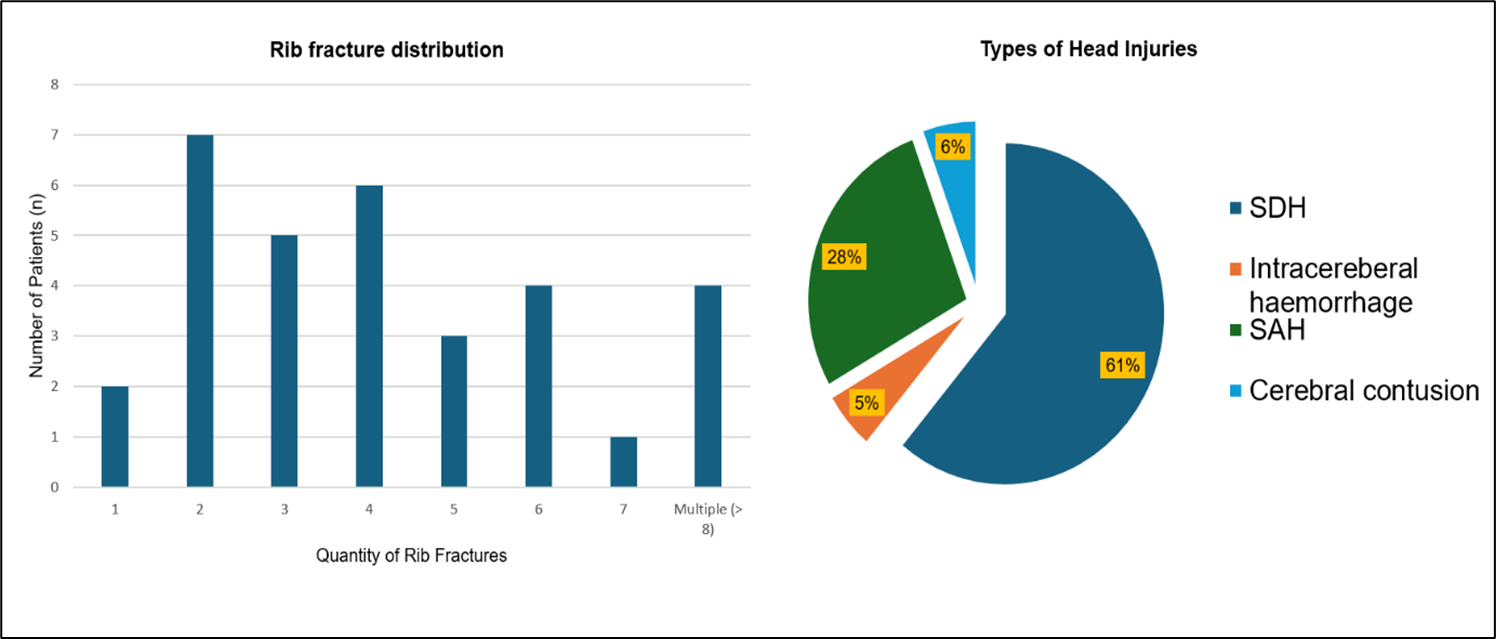
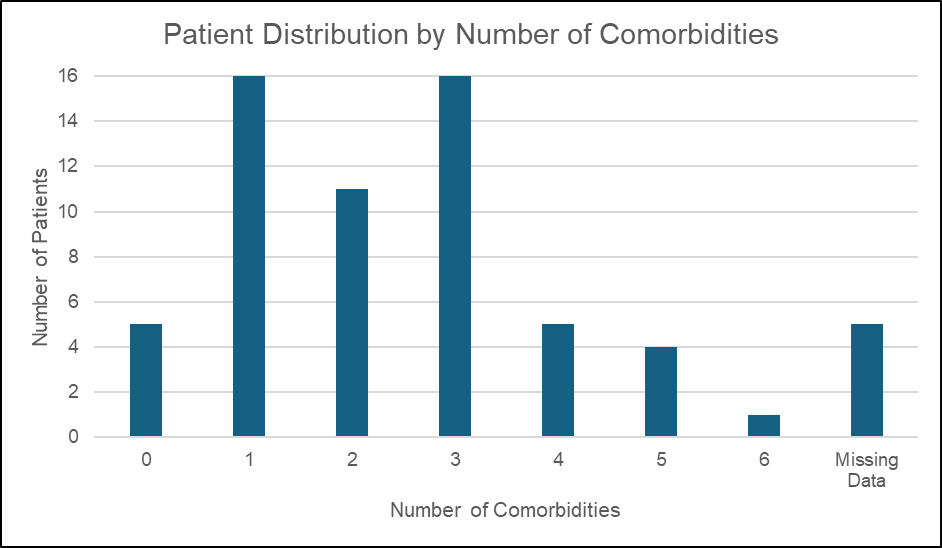
Sixty three patients were included in this study with a median age of 84 years (67–97) as shown in Figure 1a. Patients were grouped into 4 categories: Thoracic injuries, Abdominal/Pelvic (AP) injuries, Head injuries, and Multisystem injuries (i.e. ≥ 2 injuries). Thirty six patients were grouped into thoracic injuries (rib fractures, sternal fractures, and lung injuries), four patients were grouped into AP, twenty one grouped into head injuries, and two for multisystem injuries. Figure 1b shows the distribution of head injuries and the distribution of rib fractures with most patients having between 2–4 rib fractures. Subdural hematomas comprised the majority of head injuries (61%) whereas intracerebral bleeds were the least common (5%). Sixty of the sixty five analyzed patients had pre-existing comorbidities. As observed in Figure 1c, most patients had between 1–3 comorbidities, with a median of 2 comorbidities. Thirty seven patients had comorbidities limited to one body system. Of these, 20 were cardiovascular, 3 were vascular, 1 was respiratory, 2 were metabolic, and 1 was renal. The remaining patients had comorbidities affecting ≥2 body systems. The majority of these included a cardiovascular component (15 patients) followed by a renal comorbidity (3 patients).
Figure 1a. Age distribution. A scatter graph to show the age distribution. Ages ranged from 67–97 with a median age of 84 years.
Figure 1b. Of 36 patients in the Thoracic group 32 had rib fractures, 1 had a pneumothorax only, and 3 had sternal fractures only. Most patients had between 2–4 rib fractures. Of the 21 patients with head injuries 18 had an intracranial bleed, 1 had a cerebral contusion only, and 2 had cranial fractures only. Most patients had SDH (61%) and the least common group was intracerebral hemorrhage.
Figure 1c. Concurrent comorbidities. Only 5 of the patients analyzed had no concurrent medical comorbidities. The median number of comorbidities was 2.
Injury
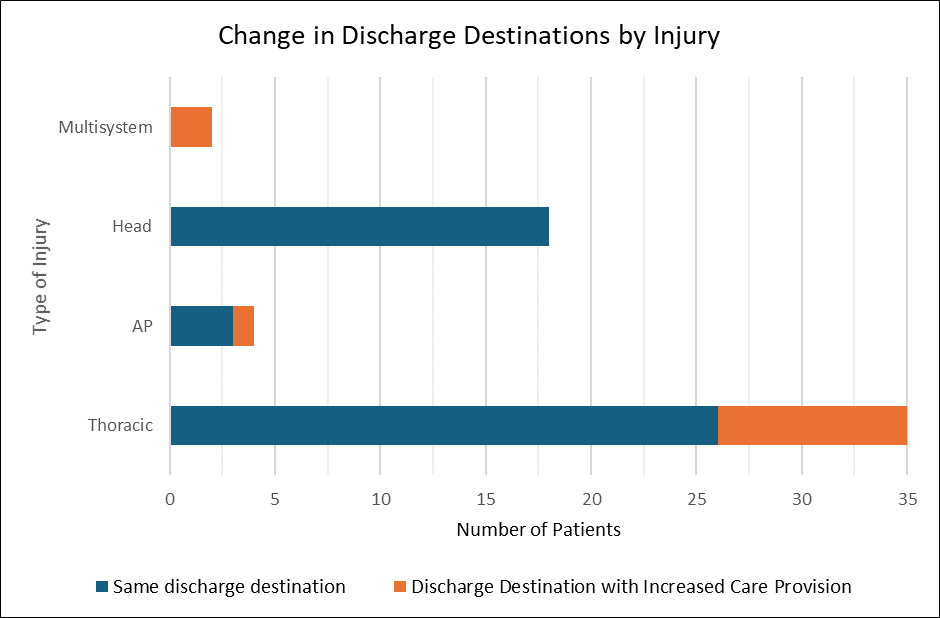
Analysis then focused on assessing the type of injury and its effect on LOS and DD. As observed in Figure 2a, patients with multisystem injuries had the highest mean LOS at 29 days (5.6), in comparison to patients with head injuries who had a mean LOS of 6.6 days (8.7). We then assessed whether injury type affected discharge destination. Of the 36 patients in the thoracic group, 9 (25%) were discharged to a destination representing reduced functional status (6 to inpatient rehab, 2 to a nursing home, and 1 to a care home). Of the 4 patients in the AP group 1 (25%) was discharged to inpatient rehabilitation and the remaining 4 patients maintained their baseline function. Interestingly all patients with head injuries were discharged to the same destination as on admission. Patients with multisystem injuries again performed the worst with 100% of patients being discharged to facilities with increased care provision (1 to inpatient rehab and one to a care home). The above is depicted below in Figure 2b.
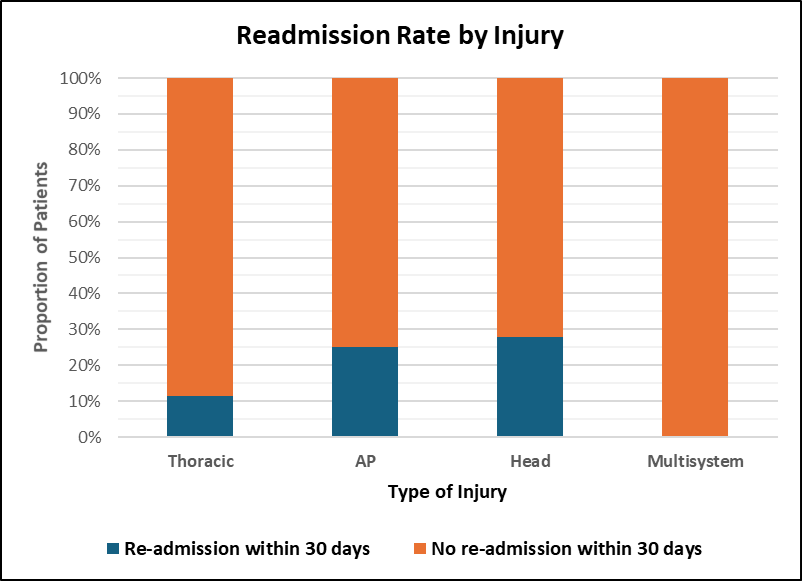
Our group then assessed the impact of injury on readmission rates. As expected, given average LOS rates, no patients with multisystem injuries had a readmission within 30 days. Four patients with thoracic injuries were readmitted in 30 days, 1 in the AP group, and 5 patients with head injuries were readmitted within 30 days, as evidenced in Figure 2c.
Figure 2a. Mean LOS by injury. As expected, patients with multisystem injuries had the greatest mean LOS at 29 days. Patients with Thoracic injuries had a mean LOS at 11.5 days, AP injuries had a mean LOS at 10.8 and patients with Head injuries had the lowest LOS at 6.6 days.
Figure 2b. Change in discharge destination by injury. All patients with multisystem injuries were discharged to destinations with less independence than on arrival. All patients with head injuries were discharged to the same destination as on arrival.
Figure 2c. Readmission rates by injury. No patients in the multisystem group had a readmission within 30 days, although this is due to their average LOS often surpassing this. Four patients with thoracic injuries were readmitted in 30 days, 1 in the AP group, and 5 patients with head injuries were readmitted within 30 days.
Nutrition
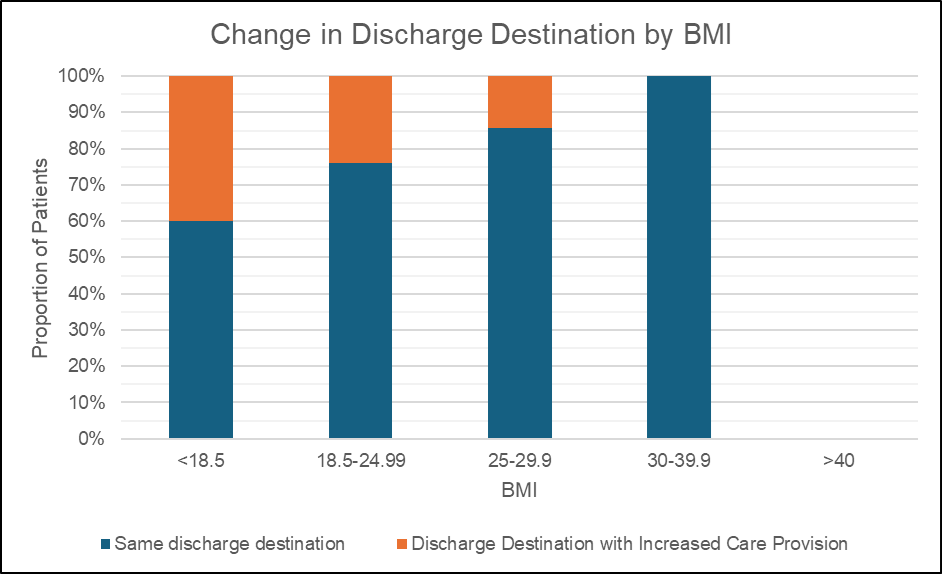
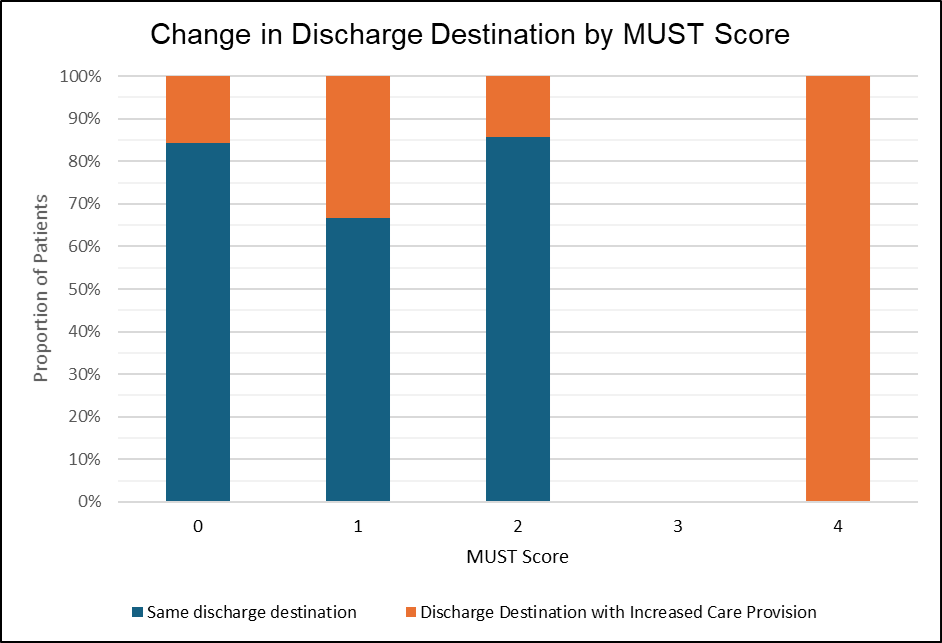
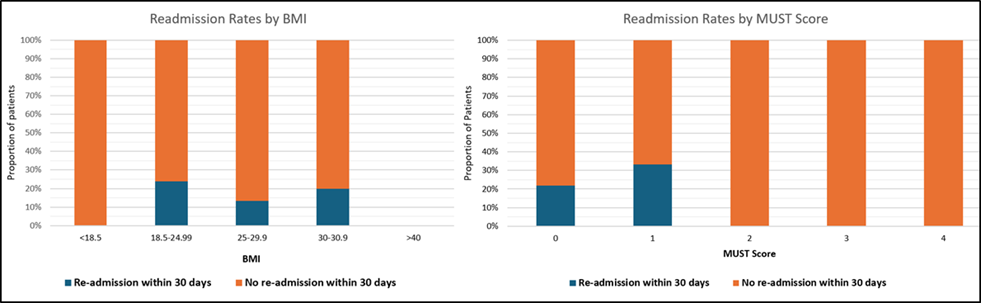
Nutrition/BMI: We then evaluated the role of nutritional status (as evidenced by MUST score) and BMI in LOS, DD, and readmission rates. As seen below in Figure 3a, patients with a BMI of <18.5 had the longest mean LOS at 18.5 days (15.3). Patients with a BMI of 18.5–24.99 had a mean LOS of 11 days (9.6), those with a BMI of 25–29.9 had a mean LOS of 13.9 days (12.7) and finally those with a BMI between 30–39.9 had a mean LOS of 4.6 days (3.4). Patients with a MUST score of 0 had the shortest mean LOS at 9.8 days (10.2), patients with a MUST score of 1 had a mean LOS of 19 days (3.1), patients with a MUST score of 2 had a mean LOS of 16.3 days (13.1), patients with a MUST score of 3 had a mean LOS of 41 days and finally those with a MUST score of 4 had a mean LOS at 13.5 days (6.4). Further analysis reinforced our findings that patients with a lower BMI (i.e. <18.5) also had worse prognostic outcomes in comparison to those with normal BMI. As evidenced in Figure 3b, patients with optimal BMI’s, had better discharge outcomes with preserved functional outcomes. The importance of nutrition was again further highlighted by assessing DD by MUST scores. All patients with a MUST score of 4 had a reduction in functional independence on discharge with all patients discharged to either a care home or nursing home, as seen in Figure 3c. 15.6% (36%) of patients with a MUST score of 0 ended up with a reduction in functional outcome, 50% (47%) for those with a MUST score of 1, 16% (33%) for those with a MUST score of 2 and 100% of those with a MUST score of 4. Finally, we assessed readmission rates by both BMI and MUST scores. However, as observed below in Figure 3d, there was no clear correlation between readmission rates and BMI or MUST scores.
Figure 3a. Mean LOS by BMI and MUST score. Patients with a BMI of <18.5 and a MUST score of 3 on average had the longest LOS (18.5 and 41 days respectively).
Figure 3b. Change in discharge destination by BMI. Patients with a BMI <18.5 had the worst functional outcomes, with 67% of patients discharged to destinations with less functional independence compared to admission.
Figure 3c. Change in discharge destination by MUST score. 100% of patients with a MUST score of 4 had a reduction of functional independence compared to those with more optimal MUST scores.
Figure 3d. Readmission rates by BMI/MUST. Our data showed no correlation between readmission rates, BMI or MUST scores.
Discussion
Given the combination of an ageing population and rising rates of trauma, the importance of optimizing care for Silver Trauma patients is essential. Silver Trauma frameworks significantly improve patients’ LOS, quality of life on discharge, and reduce morbidity and mortality. With the incidence of trauma continually rising, identifying positive prognostic indicators is now of great importance. The aim of this analysis was to identify factors that influence LOS, DD, and readmission rates. In particular we wanted to focus on 2 key areas. 1) Type of Trauma and; 2) Nutritional Status/BMI and associated outcomes. We are aware of the limitations of grouping patients, however we felt that this was the most accurate way to proceed with data analysis given the variability of injuries. The results show that, across all domains, patients with multisystem injuries have the worst prognosis. This identifies and highlights the importance and need for specialist tertiary centers equipped in managing these complex multisystem injuries. Patients with multisystem injuries, on average, had a LOS three times greater than all other injury groups in our study (Figure 2a). Patients with multisystem injuries also had the worst outcomes in terms of DD representing a decreased functional status following injury (Figure 2b). Our results support the need for major trauma centers (MTC) in the management of patients with multisystem injuries. This is supported by Moran et al., who analyzed the outcomes of major trauma patients over a 10-year period in MTCs and found that there was an increase of 0.08 more survivors per 100 patients every quarter [8]. There still remains much debate on which patients benefit from expedited MTC care; our results suggest that any patient with ≥2 anatomical injuries would greatly benefit from MTC care. When assessing readmission rates by injury, patients with head injuries had the highest proportion of readmission in comparison to other injury groups. Further analysis revealed that a higher than expected proportion of these, were patients presenting for advice, as opposed to having further complications or sequalae of their original injury. The 2014 National Readmission database described a significant readmission rate of 8.9% in patients who have sustained head injuries [9]. Identifying high risk patients may help to reduce to readmissions. Multiple studies have identified that males >80 years with a lower injury severity score account for up to 40% of these readmissions [10]. Our results show that BMI plays a significant role in outcomes of Silver Trauma patients. Patients classified as underweight (i.e. BMI <18.5) had the longest mean LOS at 18.5 days. Indeed, several studies support our findings—a large 6-year analysis between 2011 and 2017 showed that patients with a BMI <18.5 had the longest LOS and also highest mortality risk amongst surgical patients [11]. We do note however a lack of studies when comparing outcomes by BMI in Silver Trauma patients. One particular study focusing solely on trauma patients by BMI found that underweight patients had increased odds of mortality, whilst being overweight had a protective effect [12], echoing the findings of this study (Figure 3a). The early identification, recognition, and optimization of at risk, underweight patients may significantly help improve LOS and mortality rates. When assessing nutritional status by MUST scores; our results show that higher risk patients, with MUST scores of >3 have a longer LOS (Figure 3a). Early dietician and nutritional input are likely to improve prognosis for these patients. Analyzing functional status on discharge by BMI/MUST scores again reiterated that underweight, malnourished patients had a worse prognosis across all domains. Patients with a BMI <18.5 had the greatest reduction in functional status on discharge (Figure 3b) All patients with MUST scores of 4 were discharged to destinations with less functional independence compared to admission. Our study did not reveal any correlation in readmission rates by BMI/MUST scores although we note that most multisystem injury patients had LOS close to or exceeding 30 days (Figure 2a).
Conclusion
Our study has identified two groups that have worse outcomes across all domains in silver trauma—patients with multisystem injuries and underweight, malnourished patients have the least favorable outcomes in terms of LOS and functional status on discharge. Our paper highlights the importance of MTC’s in the management of multisystem injuries. Our paper also recognizes the need for early involvement of dietetics and nutritional teams, to support improved outcomes in underweight and malnourished patients. Our paper found no clear correlation between these groups and re-admission rates.
Ethics
Ethical permission was not needed for this study.
Acknowledgements
The authors acknowledge Lucy Norman and Arul Arulpragasan who helped with data collection.
Financial Support and Sponsorship
No funding was received.
Conflicts of interest
There were no conflicts of interest.
References
2. Kehoe A, Smith JE, Edwards A, Yates D, Lecky F. The changing face of major trauma in the UK. Emerg Med J. 2015 Dec;32(12):911–5.
3. National Audit Office. Major Trauma Care in England. HC 213, 2009–2010. Executive Summary. London, UK: The Stationery Office; 2010.
4. Murali M, Bolton L, Bhaktal S77 Silver trauma pathway: a new gold standard in elderly trauma care BMJ Leader 2018;2:A32.
5. NHS Scotland. Silver trauma. Right Decisions website. Accessed October 10, 2025. Available from:https://rightdecisions.scot.nhs.uk/south-east-scotland-major-trauma-guidelines/reception-resuscitation/silver-trauma/.
6. Royal College of Emergency Medicine. RCEM Safety Alert – Silver Trauma. Published September 2019. Accessed October 10, 2025. Available from: https://rcem.ac.uk/wp-content/uploads/2021/10/RCEM_safety_alert_Silver_Trauma_Sept_2019.
7. Haines M, Measey MM, Whitty A, McCoy N, McCabe A. Demographics, management and outcomes of major trauma in older patients at an Irish trauma unit. Ir J Med Sci. 2025 Feb;194(1):347–51.
8. Moran CG, Lecky F, Bouamra O, Lawrence T, Edwards A, Woodford M, et al. Changing the System - Major Trauma Patients and Their Outcomes in the NHS (England) 2008-17. EClinicalMedicine. 2018 Aug 5;2-3:13–21.
9. NHS England Digital. Emergency Readmissions Within 30 Days of Discharge from Hospital – Specification v5.0 (I02040 & I00712). Published 2020. Accessed October 10, 2025.Available from: https://digital.nhs.uk/data-and-information/publications/statistical/nhs-outcomes-framework.
10. Pilkington C, Thind T, Bowman SM, Sexton K, Kimbrough MK, Porter A, et al. Readmissions After Traumatic Brain Injury in the Nationwide Readmissions Database. J Surg Res. 2024 Jun;298:36–40.
11. Dotan I, Shochat T, Shimon I, Akirov A. The Association Between BMI and Mortality in Surgical Patients. World J Surg. 2021 May;45(5):1390–9.
12. Dvorak JE, Lester ELW, Maluso PJ, Tatebe L, Schlanser V, Kaminsky M, et al. The Obesity Paradox in the Trauma Patient: Normal May not Be Better. World J Surg. 2020 Jun;44(6):1817–23.