Abstract
Introduction: Sentinel node biopsy is currently the standard of care for axillary treatment of clinically axillary node-negative breast cancer. In this report, we describe a case of axillary lymph node recurrence 10 years after surgery in a patient with a negative sentinel node biopsy at the time of initial surgery.
Presentation of case: The patient was a 49-year-old premenopausal woman. She had undergone left mastectomy and sentinel node biopsy (dye method only) for left breast cancer (T3N0M0) 10 years earlier. Ten years after surgery, an enlarged left axillary lymph node measuring 2 cm in diameter was noted on ultrasound examination. Left axillary lymph node dissection was performed. Postoperative histopathology showed that the tumor cells were negative for E-cadherin and that the patient had invasive lobular carcinoma.
Discussion: A second sentinel node might have been missed considering that the sentinel node was detected by the dye method alone, without use of the isotope method, which might have enabled detection of another sentinel node. Observation of the axillary lymph nodes is essential for follow-up after sentinel node biopsy.
Conclusion: After sentinel node biopsy, postoperative follow-up imaging studies should include ultrasonography to check for enlarged lymph nodes.
Keywords
Breast cancer, Sentinel lymph node, False negative, Late recurrence
Introduction
Sentinel node biopsy is currently the standard of care for axillary treatment of clinically axillary node-negative breast cancer. According to a report on the long-term results of sentinel node-negative patients from whom axillary lymph node dissection was omitted, the rate of axillary lymph node recurrence is less than 1%. The time to recurrence is most frequently within 2 years after surgery. In this report, we describe a case of axillary lymph node recurrence 10 years after surgery in a patient with a negative sentinel node biopsy at the time of initial surgery. This report was written in accordance with the SCARE criteria [1].
Presentation of Case
The patient was a 49-year-old premenopausal woman. She had undergone left mastectomy and sentinel node biopsy for left breast cancer (T3N0M0) 10 years earlier. Sentinel node biopsy was performed using the dye method alone. Histopathology revealed invasive ductal carcinoma of the breast and scirrhous carcinoma, which were estrogen receptor positive, progesterone receptor positive, and HER2 negative. No sentinel node metastasis was detected (0/1).
Because of positive breast margins, she received systemic chemotherapy with anthracycline, cyclophosphamide, and paclitaxel. She also underwent postmastectomy radiation therapy with a total dose of 50 Gy. She then received tamoxifen and luteinizing hormone-releasing hormone agonist until 9 years postoperatively. Regular local examinations were performed, including annual ultrasound examinations.
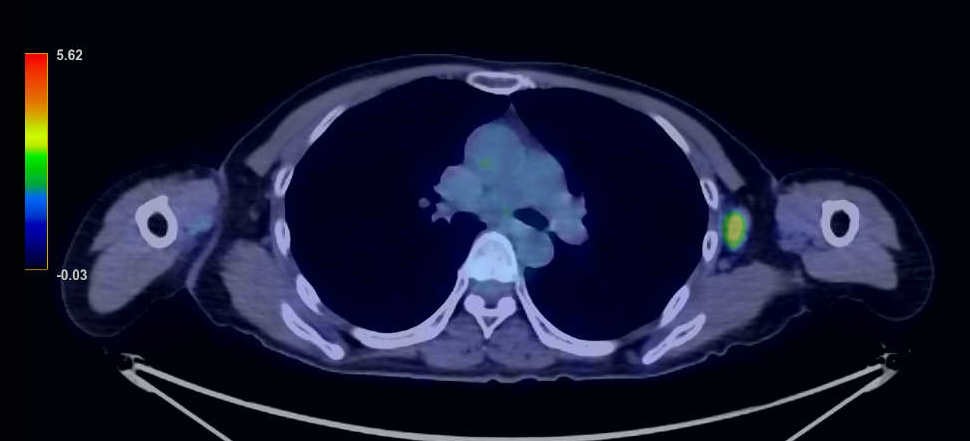
During a routine postoperative ultrasound examination 10 years after surgery, an enlarged left axillary lymph node measuring 2 cm in diameter was noted (Figure 1). A needle biopsy of the enlarged lymph node was performed, and metastatic recurrence of breast cancer was diagnosed. The histopathology of the needle biopsy showed highly attenuated expression of E-cadherin, which suggested the possibility of invasive lobular carcinoma. CT and PET/CT scans showed only enlarged left axillary lymph nodes and no distant metastasis (Figures 2 and 3).


Figure 1. Ultrasound image showing an enlarged lymph node in the left axilla. It is 23 mm in diameter and at least two nodes can be seen.
Figure 2. CT scan showing an enlarged lymph node in the left axilla. No obvious metastases are seen in other organs.
Figure 3. PET/CT scan showing a left axillary lymph node with a maximum standard uptake value of 3.7. No accumulation is seen in other organs.
The left axillary lymph node dissection was performed for the axillary lymph node recurrence. Postoperative histopathologic examination revealed lymph node metastasis (17/17) that was estrogen receptor positive, progesterone receptor negative, and HER2 positive (2+), with Ki-67 20% and no FISH amplification. The tumor cells were E-cadherin negative and were diagnosed as invasive lobular carcinoma.
Seven courses of docetaxel and cyclophosphamide were administered as postoperative chemotherapy. The patient was followed up with outpatient visits, but 18 months after surgery, headache and nausea appeared. A head MRI was performed, and multiple brain metastases were diagnosed. Whole-brain irradiation was performed for the brain metastases.
She was treated with eribulin, bevacizumab, and paclitaxel, but developed carcinomatous meningitis and died 2 years and 5 months after the axillary dissection surgery.
Discussion
Sentinel node biopsy is the current standard of care for clinically axillary node-negative breast cancer and has the following benefits: (1) accurate staging is possible, (2) it can also be used as treatment of the axilla, and (3) it is much less invasive than axillary dissection.
The dye and isotope methods are mainly used to identify sentinel lymph nodes, and the identification rate is reported to be 97-98%. The combined use of both methods is considered optimal, but the dye method alone has been reported to be comparable, with a false-negative rate of 5% [2].
The frequency of axillary recurrence after sentinel node biopsy is 0.25-0.9% and is often reported to be less than 1% (observation period 26-75 months) [3-5]. This is much lower than the recurrence rate expected based on false negative rates [6-8]. Recurrence is most common within 2 years after surgery [1]. Sentinel node biopsy is now widely used, and the recurrence rate may increase with longer observation periods, but there have been few reports on the results of sentinel node biopsy in recent years. Most cases of axillary recurrence have multiple metastases, and metastasis in a single axillary lymph node is rare. It is estimated that 30% of patients with axillary recurrence have distant metastases.
The most likely reason for the axillary lymph node recurrence in this case was that a second sentinel node was missed at the time of the initial surgery (i.e., a false negative) [9]. This might have occurred because the dye method alone was used to identify the sentinel node at the time of the initial surgery, without use of the isotope method. It is possible that another sentinel node could have been identified if the isotope method had been used.
However, if metastasis had already occurred, it is possible that tumor cells obstructed the lymphatic vessels, and that dye could not migrate to the second sentinel node. Whether identification would have been possible is a matter of speculation.
The late recurrence 10 years after surgery is assumed to be due to suppression of tumor cell proliferation by postoperative radiotherapy, chemotherapy, and hormone therapy. However, these multidisciplinary therapies failed to destroy the tumor cells, and surgical excision of metastatic lymph nodes is still considered the best method of preventing axillary recurrence.
Treatment of axillary recurrence requires additional axillary lymph node dissection followed by systemic chemotherapy. In this case, the patient had an adverse outcome due to distant recurrence despite the use of aggressive postoperative chemotherapy. One of the reasons for the late recurrence and the poor outcome may have been that the ductal carcinoma at the time of the initial surgery had transformed into lobular carcinoma on histopathological examination after the recurrence.
A high axillary recurrence rate has been reported in patients with hormone receptor-negative disease, triple negative breast cancer, mastectomy, and no adjuvant radiation therapy [1]. Although this patient had undergone mastectomy, she received postoperative radiation and did not appear to be at high risk for recurrence. Observation of axillary lymph nodes is still essential for follow-up after sentinel node biopsy.
Both mammography and ultrasound examination of the breast are considered effective. However, late recurrence is not common, and it is difficult to determine how long postoperative follow-up should be continued.
Conclusion
We encountered a case of sentinel node biopsy-negative breast cancer with axillary lymph node recurrence 10 years after the initial surgery. Postoperative follow-up imaging studies should include ultrasonography to check for the presence of enlarged lymph nodes.
Consent
Written informed consent was obtained from the patient’s family for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical Approval
Our institution does not require ethical approval for case reports that are deidentified and written retrospectively. Ethical approval was waived by the authors’ institution.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Provenance and Peer Review
Not commissioned, externally peer-reviewed.
Declaration of Competing Interests
None.
Acknowledgments
Not applicable.
References
2. Nakajima H, Fujiwara I, Mizuta N, Sakaguchi K, Hachimine Y, Nakatsukasa K, et al. Axillary lymph node recurrence after negative sentinel lymph node biopsy for breast cancer. J Jpn Surg Assoc. 2008;69(8):1866-71.
3. Smidt ML, Janssen CM, Kuster DM, Bruggink ED, Strobbe LJ. Axillary recurrence after a negative sentinel node biopsy for breast cancer: incidence and clinical significance. Annals of Surgical Oncology. 2005 Jan;12:29-33.
4. Ogiya A, Kimura K, Nakashima E, Sakai T, Miyagi Y, Iijima K, et al. Long-term prognoses and outcomes of axillary lymph node recurrence in 2,578 sentinel lymph node-negative patients for whom axillary lymph node dissection was omitted: results from one Japanese hospital. Breast Cancer. 2016 Mar;23:318-22.
5. Van der Ploeg IM, Nieweg OE, Van Rijk MC, Olmos RV, Kroon BB. Axillary recurrence after a tumour-negative sentinel node biopsy in breast cancer patients: a systematic review and meta-analysis of the literature. European Journal of Surgical Oncology (EJSO). 2008 Dec 1;34(12):1277-84.
6. Roumen RM, Kuijt GP, Liem IH, Van Beek MW. Treatment of 100 patients with sentinel node‐negative breast cancer without further axillary dissection. British Journal of Surgery. 2001 Dec;88(12):1639-43.
7. Veronesi U, Paganelli G, Viale G, Luini A, Zurrida S, Galimberti V, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. New England Journal of Medicine. 2003 Aug 7;349(6):546-53.
8. Naik AM, Fey J, Gemignani M, Heerdt A, Montgomery L, Petrek J, et al. The risk of axillary relapse after sentinel lymph node biopsy for breast cancer is comparable with that of axillary lymph node dissection: a follow-up study of 4008 procedures. Annals of Surgery. 2004 Sep 1;240(3):462-8.
9. Motomura K, Egawa C, Komoike Y, Hasegawa Y, Koyama H, Inaji H. Axillary recurrence after negative sentinel node biopsy in a patient with breast cancer: Report of a case. Surgery Today. 2006 Mar;36:267-9.