Abstract
Here, we report a 26-year-old Chinese woman diagnosed with breast cancer. The patient expressed her concern for possible impact on fertility, as well as the cosmetic outcomes of the surgery. Therefore, the patient was consulted for preserving fertility function by cryopreservation after ovariectomy, with sentinel lymph node biopsy and breast reconstruction surgery simultaneously.
With the development of health care and the growth of economy, as well as the general awareness of full-round health, the need for reproductive preservation of young female breast cancer patients in developing countries is also increasing. Thus, we recommend actively providing patent education for the reproductive protection operation on a regular basis, to reduce the cases of patients who suffer from a decline in fertility.
Keywords
Fertility, Fertility-sparing, Breast cancer, Reproductive protection operation
Introduction
Breast cancer is the most common female cancer in the world [1]. 11% of breast cancer patients are younger than 45 years old [2]. More and more researchers begin to pay attention to how to retain the patient fertility while treating breast cancer. It also helps improve the quality of life for young female breast cancer patients. Therefore, the reproductive need of young female breast cancer patients starts to play a pivotal role in the treatment and recovery of breast cancer.
Studies have shown that radiotherapy and chemotherapy for breast cancer increase the risk of gonadal failure [3]. Among adolescent women with cancer, 81% patients and 93% parents of the patients are interested in preserving fertility, even if such fertility preserving techniques are still experimental [4]. Our team performed several fertility-sparing surgical operations to maintain the fertility of patients. The ovarian tissue is resected and preserved for future transplantation while breast cancer is being treated. This procedure has been reported in the Danish [5], Australia [6], etc. but we have not found any relevant surgical reports in the developing countries. This case report is the first reported breast cancer fertility-sparing surgery in Asia and developing countries.
Case Report
A 26-year-old female presented with bloody nipple discharge on left side. After being diagnosed with invasive breast cancer by puncture biopsy (Figure 1), the patient expressed her concern for possible impact on fertility, as well as the cosmetic outcomes of the surgery. Therefore, the patient was consulted for preserving fertility function by cryopreservation after ovariectomy, with sentinel lymph node biopsy and breast reconstruction surgery simultaneously. The patient consented for the treatment plan. with minor rearrangements to allow SEB to bind to CD28.
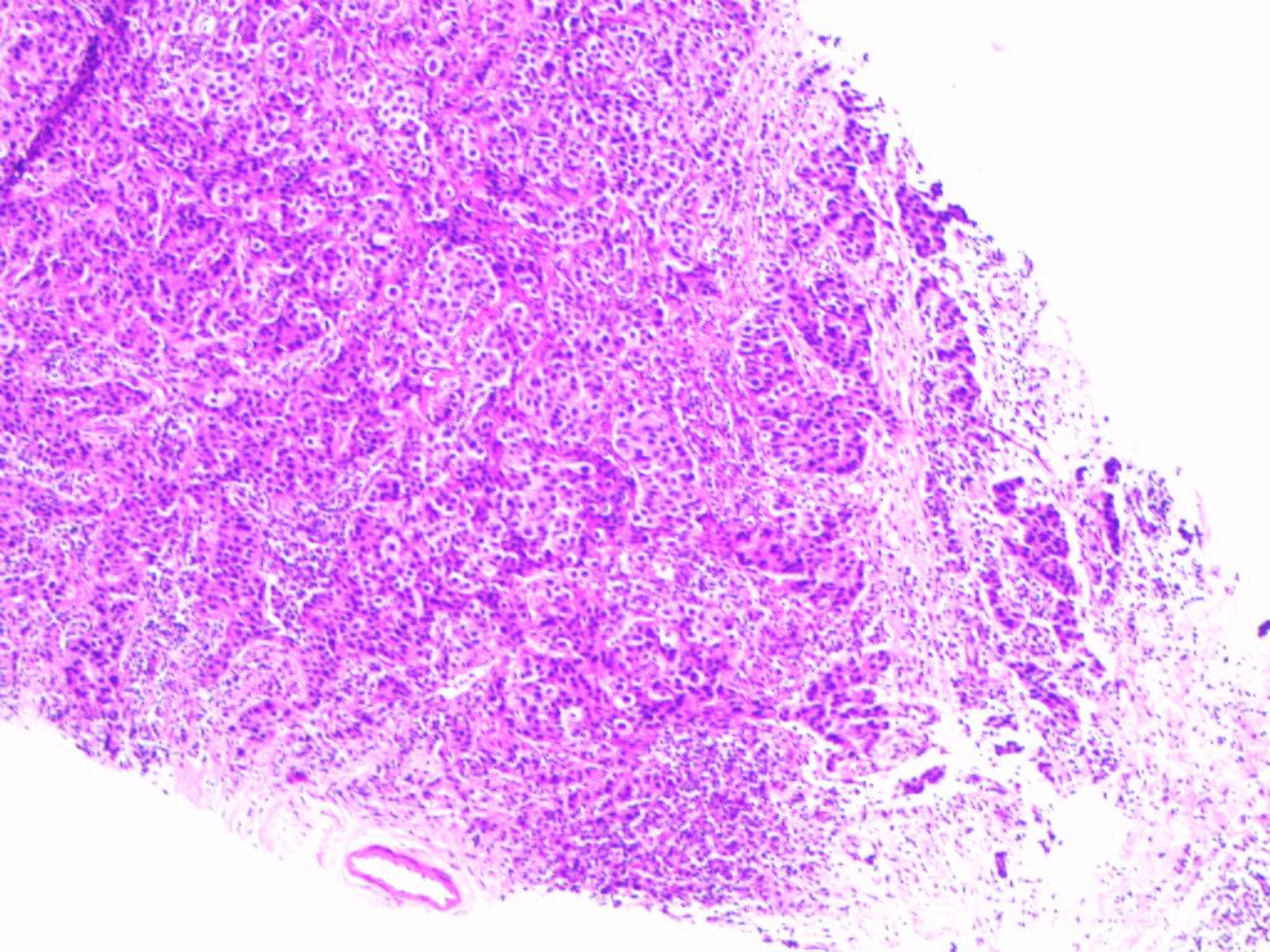
Figure 1: The arrangement of cancer cells showed irregular cell clusters and overlapping nuclei, showing atypia. Chromatin increased significantly. Multiple red-stained punctate necrosis can be seen.
After induction of general anesthesia, methylene blue and carbon nanoparticles were injected into the left areola of the patient. Then the sentinel lymph nodes and the incision margin of the base of the nipple were taken for rapid pathology. Pathological findings showed no metastasis. Therefore, we performed left mastectomy without lymph node dissection. After implantation of breast prosthesis for breast reconstruction, incision suture was used. Next, we re-disinfect the towel and established a pneumoperitoneum. No obvious abnormalities were found in the uterus and its appendages. A wedge-shaped resection of a small amount of right ovarian tissue was performed (Figure 2), and the resected tissue was cryopreserved in liquid nitrogen. Then the resected ovarian tissue was sent to pathology and storage. The patients recovered well after operation and no discomforts nor complications were found during follow-ups.
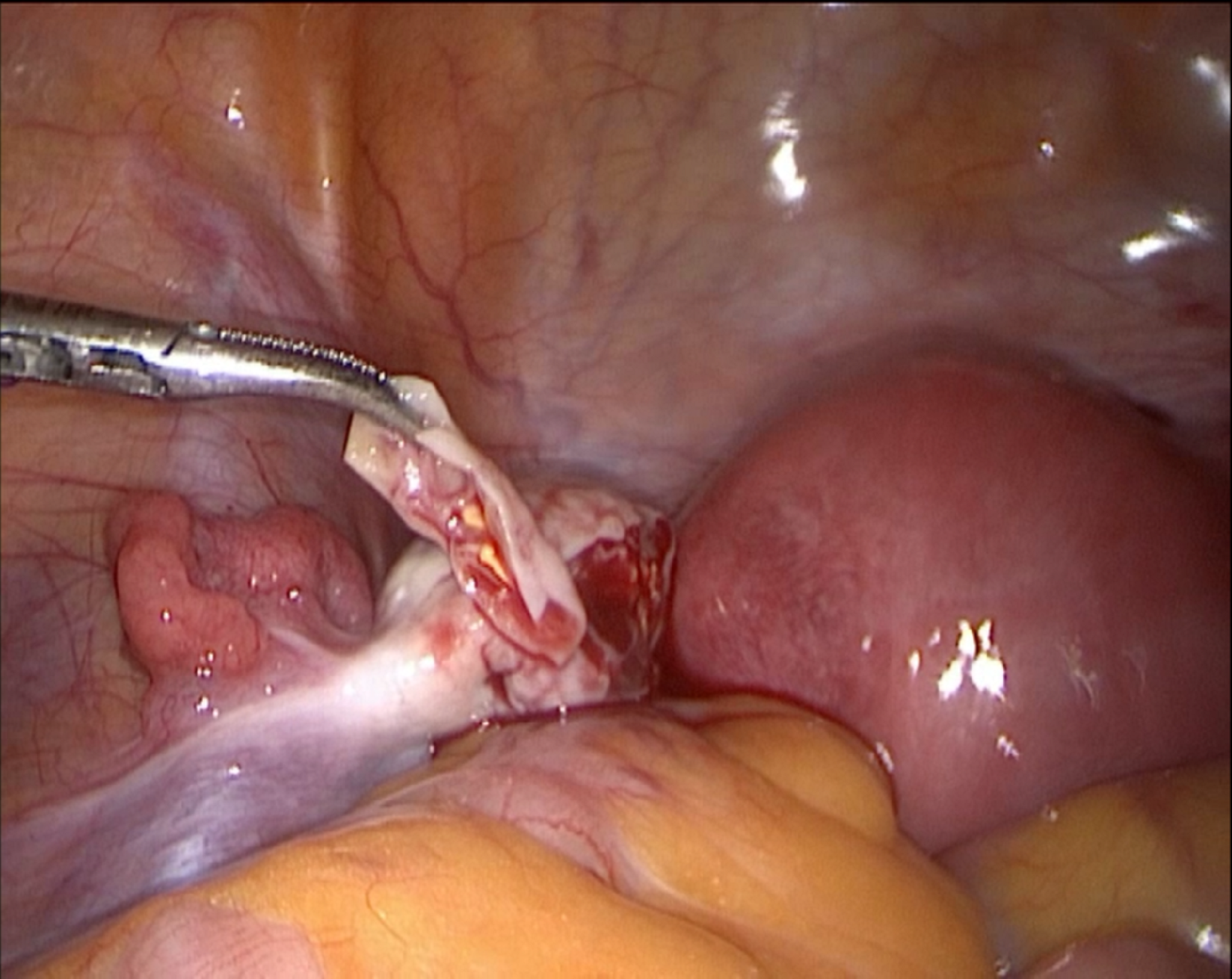
Figure 2: Laparoscopic ovarian wedge resection.
Discussion
The main cause of ovarian damage or premature ovarian failure in cancer patients is the use of anticancer drugs. And this could lead to irreversible damage in some cases. Cyclophosphamide plays a major role in ovarian chemotherapy injury [7]. A study has reported that cyclophosphamide destroys ovarian reserve mainly by activating primordial follicles, thereby accelerating the consumption of follicles [8]. Some researchers also believe that cyclophosphamide can reduce estrogen and progesterone levels, and can cause fibrosis of the ovary [9]. However, as a common alkylating agent, the presence of cyclolinamide is indispensable in most breast cancer chemotherapy regimens.
For fertility-sparing surgery, most of the current research focuses on ovarian and cervical cancer. Although in recent years, some researchers have proposed that a new guideline is needed for the fertility preservation of young breast cancer patients [10], research on the reproductive needs of premenopausal breast cancer patients are of limited number. Among them, ovarian tissue cryopreservation is recommended as a fertility preservation technology. The application of such fertility preservation in breast cancer surgery is very important. For patients with frozen ovarian tissue, ovarian tissue transplantation can be performed after chemotherapy and before fertility is required. Regarding the risk of malignant tumor cell replantation during autologous tissue transplantation, a retrospective study of follow-up after autologous transplantation showed that in 289 cases collected by researchers, breast cancer patients did not see metastatic diseases after ovarian transplantation [11].
With the economic growth of developing countries, the demand for cancer treatment is changing from a simple need for survival to a need for both survival and quality of life. Our health care team realized this increasing need of our young female breast cancer patients. Therefore, we started to provide fertility protection counseling on a regular basis. We also found that many young female breast cancer patients do have this need, however, most of them are not aware of the possibility for preserving fertility. As a result of patient education, many early breast cancer patients who wish to preserve their fertilities have undergone the same surgery in our team.
In conclusion, with the increasing number of young female breast cancer patients, we should take into account that the reproductive needs of young patients while treating breast cancer. With the development of health care and the growth of economy, as well as the general awareness of full-round health, the need for reproductive preservation of young female breast cancer patients in developing countries is also increasing. Thus, we recommend actively providing patent education for the reproductive protection operation on a regular basis, to reduce the cases of patients who suffer from a decline in fertility.
Contributors
Drafting of the manuscript was performed by Cunye Yan. Critical revision was performed by Chenyu Sun. Benzhong Wang conceived and finally reviewed the manuscript. All the authors were involved in the operation.
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.
References
2. American Cancer Society. Cancer facts & figures. The Society; 2008.
3. Goodwin PJ, Ennis M, Pritchard KI, Trudeau M, Hood N. Risk of menopause during the first year after breast cancer diagnosis. Journal of Clinical Oncology. 1999 Aug 1;17(8):2365-70.
4. Burns KC, Boudreau C, Panepinto JA. Attitudes regarding fertility preservation in female adolescent cancer patients. Journal of Pediatric hematology/oncology. 2006 Jun 1;28(6):350-4.
5. Ernst EH, Offersen BV, Andersen CY, Ernst E. Legal termination of a pregnancy resulting from transplanted cryopreserved ovarian tissue due to cancer recurrence. Journal of Assisted Reproduction and Genetics. 2013 Jul 1;30(7):975-8.
6. Burmeister L, Kovacs GT, Osianlis T. First Australian pregnancy after ovarian tissue cryopreservation and subsequent autotransplantation. Medical Journal of Australia. 2013 Feb 18;198(3):158-9.
7. Welt C, Shapiro C, Crowley Jr WF. Ovarian failure due to anticancer drugs and radiation. UpToDate version. 2010 Sep;18.
8. Kalich-Philosoph L, Roness H, Carmely A, Fishel-Bartal M, Ligumsky H, Paglin S, et al. Cyclophosphamide triggers follicle activation and “burnout”; AS101 prevents follicle loss and preserves fertility. Science translational medicine. 2013 May 15;5(185):185ra62.
9. Oktay K, Sönmezer M. Chemotherapy and amenorrhea: risks and treatment options. Current Opinion in Obstetrics and Gynecology. 2008 Aug 1;20(4):408-15.
10. Shah NM, Scott DM, Kandagatla P, Moravek MB, Cobain EF, Burness ML, Jeruss JS. Young women with breast cancer: fertility preservation options and management of pregnancy-associated breast cancer. Annals of Surgical Oncology. 2019 May 15;26(5):1214-24.
11. Bastings L, Beerendonk CC, Westphal JR, Massuger LF, Kaal SE, Van Leeuwen FE, et al. Autotransplantation of cryopreserved ovarian tissue in cancer survivors and the risk of reintroducing malignancy: a systematic review. Human Reproduction Update. 2013 Sep 1;19(5):483-506.
