Abbreviations
CABG: Coronary Artery Bypass Graft surgery, CTO: Chronic Total Occlusion, IS-CTO = In-Stent Chronic Total Occlusion, PCI: Percutaneous Coronary Intervention, J-CTO: Japanese Chronic Total Occlusion score, IVUS: Intravascular Ultrasound, TVR: Target Vessel Revascularization
Introduction
As the Percutaneous Coronary Intervention (PCI) is prevalent in the recent decades, In-Stent Coronary chronic Total Occlusion (IS-CTO) has become a frequently met lesion in daily PCI procedure. It is estimated IS-CTO PCI accounts for 5-25% of all CTO [1]. Although the success rate of CTO PCI is around 90% in heart centers that are proficient with CTO PCI procedure [1], CTO remains the most time-consuming and challenging subset of lesions in all the PCI procedures. The structural differences between de novo CTO with IS-CTO were found to significantly affect the PCI success rate and prognosis. IS-CTO PCI generally achieves lower success rate of 63% to 71% [2-5]. The existence of a foreign body, implanted stent structure, negatively affects IS-CTO lesion’s long-term outcome comparing to de novo CTO. The successful IS-CTO PCI group has a surprisingly high rate of restenosis and re-occlusion (28.5%) [6]. IS-CTO has been identified as an independent predictor of Target-Vessel Revascularization (TVR) [5].
IS-CTO Scoring System
Currently, J-CTO score and progress CTO score are the most widely accepted scoring systems to evaluate the difficulty of CTO PCI procedures. However, both scoring systems fail to take the unique character of IS-CTO into consideration. It is not appropriate to be used to assess the difficulty of IS-CTO PCI. In the issue of Journal of Cardiovascular Translational Research: Gong et al. [7] developed a specific scoring model for predicting the technical success of IS-CTO. They collected 474 complex IS-CTO PCI cases, which was the largest sample of IS-CTO study to date. The overall procedural success rate was 77.4%. Besides traditional risk factors such as calcification, bending, blunt stump, occlusion length ≥ 20mm, prior failed attempts (J-CTO score), proximal cap ambiguity, quality of the distal vessel, circumflex CTO target vessel, and presence of adequate collateral vessel (PROGRESS CTO score), the author added proximal bending ≥ 30° (beta coefficient [β]=2.142), tortuosity bending ≥ 20° (β=2.622), stent under expansion (β=3.052), and poor distal target (β=2.004) as risk factors, and developed this new scoring system. IS-CTO score was superior to the J-CTO and PROGRESS CTO scores for predicting technical success.
The Specificity of IS-CTO Score
Perhaps the barriers that previously affecting the success of PCI procedures are no longer significant due to the development of new techniques, advanced devices, and training courses organized by expert operators. For example, many traditional factors (blunt stump, occlusion length ≥ 20 mm, and prior failed attempts) that affect the success ratio in de novo CTO seem to no longer be crucial in IS-CTO PCI in this study. In fact, it is true that the stent’s contour shows a good landmark and makes it easier for the operator to identify the entry point during the operation. The calcification was excluded during the development and validation of this IS-CTO score system. There are fewer calcifications involved in IS-CTO than in de novo CTO [8] in histopathology. In the IS-CTO, the intimal calcification cannot be evaluated sufficiently by angiography due to the artifact of prior implanted stents. The calcification beyond the stent had no influence on the procedure. Therefore, it is conceivable that the success ratio of IS-CTO PCI is not associated with the calcification.
The author established a significant correlation between IS-CTO PCI failure and proximal bending ≥ 30°, as well as tortuosity (bending) ≥ 20°. Of course, IS-CTO shows different characteristics comparing to de novo CTO’s bending because the implanted stent always straightens the vessels’ curvature or angle. The cut-off points were estimated by the Youden index.
Dr. Gong et al. believe stent under-expansion is another important variable in predicting IS-CTO PCI success, which is detrimental to recanalizing IS-CTO. Stent under-expansion in IS-CTO is defined as: the stent’s outline protrudes into the stent’s center from the baseline of the stent’s contour with a maximal height of more than 20% of the average reference stent diameter at any side. The cut-off point was estimated by the Youden index. This definition is used widely in angiography due to its practicality. The difficulty of wire and balloon crossing [9] determines the success rate of IS-CTO procedures. Occluded stents which were under-expanded make wiring through the occlusion much more difficult. A stent fracture, disruption of the original stent architecture, or even a metallic scaffold would block the wire’s path, especially in a tortuous vessel segment. Even after wire crossing, the balloon can still be blocked by the struts protruding into the lumen. Chronic IS-CTO lesions are often filled with hard fibrous tissue. The fibrous tissue mixed with metal struts in the occlusion segments significantly increases the technical difficulty of PCI procedures when maneuvering the wire [10], making it nearly impossible to penetrate.
The Superiority of IS-CTO Score
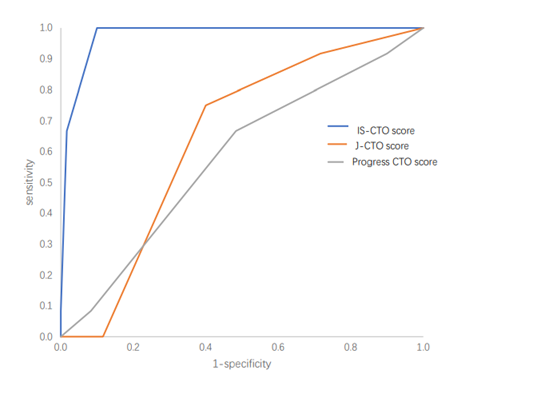
To verify the superiority of IS-CTO score in predicting the success of the procedure, the author produced the ROC curve of IS-CTO, J-CTO and progress CTO score (Figure 1), which demonstrated the excellent predictive value for IS-CTO score (area under the curve=0.976) as compared to the predictive value for PROGRESS CTO score (area under the curve=0.579) and the J-CTO score (area under the curve=0.642).
Figure 1: Receiver-operator characteristic curves of the IS-CTO score, PROGRESS CTO, and J-CTO scores in the validation Dataset. IS-CTO score (area under the curve=0.976), PROGRESS CTO score (area under the curve=0.579), and the J-CTO score (area under the curve=0.642). PROGRESS CTO: Prospective Global Registry for the Study of Chronic Total Occlusion Intervention; J-CTO: Multicenter Chronic Total Occlusion Registry in Japan; IS-CTO: In-Stent Chronic Total Occlusion.
Study Limitations
However, it is a pity that the author couldn’t provide Intravascular Ultrasound (IVUS) data, which would help to identify the lesion characteristics and mechanisms of IS-CTO. The IVUS can guide the operator in decision-making by finding the true lumen in the CTO PCI procedure, thus improve the success ratio. In-stent CTO PCI with drug-eluting stents optimized by IVUS guidance improve long-term clinical results [11]. IVUS guided PCI is correlated with better procedure and clinical outcomes in IS-CTO PCI [12].
The procedural success rate was 77.4% in the study, lower than 86.5% in published data [8]. Although nearly 30 operators were enrolled in a nondiscriminatory manner from as far back as 5 years ago, only 19 cases utilized the retrograde approach. The percentage of retrograde seemed relatively small (4%) compared to other centers proficient at CTO procedures and the predictive model was more convincing for the antegrade approach algorithm.
Pathophysiology of IS-CTO
IS-CTO could be a result of in-stent restenosis or stent thrombosis. In-stent restenosis may result from stent recoil, under-deployment or fracture that led to neointima proliferation. CTO that results from in-stent restenosis is most commonly composed of a hypocellular matrix made up primarily of hard and resistant collagenous material, and therefore differ from other CTO because of the relative absence of in-plaque micro-channels. Those soft wires are less steerable and may also slip outside the stent structure, in the sub-intimal plane. Therefore, the most useful guidewire family in that situation are high torque and hard tip wires which provide a very acute control and torque of the tip to allow the wire to stay within the stent. Mechanical factors such as poor expansion, malposition, distal dissection and poor outflow may result in acute thrombosis leading to an organized CTO.
Clinical Outcomes of IS-CTO PCI
IS-CTO has been identified as an independent predictor of TVR, it can be reasonably inferred that a patient’s biological factors are possible causes for the higher risk of re-occlusion when re-stented. These factors may include abnormal local morphology, inflammatory reaction, adverse reactions to stent polymers, antiplatelet drug resistance, under expansion/malposition, or the presence of other immune diseases. Given the high risk of TVR, it is imperative to use multimodal imaging to understand the etiology of the prior stent failure to optimize stent expansion. Additionally, longer than 18 months of dual antiplatelet therapy was an independent predictor for decreased TVR (HR: 2.682; 95% CI: 1.295–5.578 P = 0.008) [6]; To decrease major adverse cardiac events, dual antiplatelet therapy was found to be essential and recommended for at least 18 months for IS-CTO PCI. Finally, under certain circumstances such as significant concomitant LM disease, multivessel disease, more complex coronary artery disease or a high SYNTAX score Coronary Artery Bypass Graft surgery (CABG) should be considered as an initial treatment option for patients with IS-CTO. CABG may reduce the risk of TVR and give complete arterial revascularization.
Conclusions
We conclude IS-CTO should be identified as a disparate entity that carries its own characteristics. IS-CTO should be considered as a predictor of PCI failure due to its difference compared to de novo CTO. We propose IS-CTO scoring system should be taken as a predictor for technical difficulty and success rate of IS-CTO PCI.
Conflicts of Interest
The author has no conflicts of interest to disclose.
References
2. Abbas AE, Brewington SD, Dixon SR, Boura J, Grines CL, O’Neill WW. Success, Safety, and Mechanisms of Failure of Percutaneous Coronary Intervention for Occlusive Non–Drug-Eluting In-Stent Restenosis Versus Native Artery Total Occlusion. The American Journal of Cardiology. 2005 Jun 15;95(12):1462-6.
3. Wilson WM, Walsh S, Hanratty C, Strange J, Hill J, Sapontis J, et al. A novel approach to the management of occlusive in-stent restenosis (ISR). EuroIntervention. 2014 Mar 1;9(11):1285-93.
4. Werner GS, Moehlis H, Tischer K. Management of total restenotic occlusions. EuroIntervention. 2009 May;5: D79-83.
5. Abdul-rahman R, Lombardi WB, Banerjee S, Brilakis ES. Contemporary outcomes of percutaneous intervention in chronic total coronary occlusions due to in-stent restenosis. Cardiovascular Revascularization Medicine. 2011 May 1;12(3):170-6.
6. Gong ML, Mao Y, Liu JH. Long-term outcomes of percutaneous coronary intervention for in-stent chronic total occlusion. Chinese Medical Journal 2020; 134: 302-308.
7. Gong M, Peng H, Wu Z, Li W, Lv Y, Lv Y, et al. Angiographic Scoring System for Predicting Successful Percutaneous Coronary Intervention of In-Stent Chronic Total Occlusion. Journal of Cardiovascular Translational Research. 2021 Jan 6:1-2.
8. Azzalini L, Dautov R, Ojeda S, Benincasa S, Bellini B, Giannini F, Chavarría J, Pan M, Carlino M, Colombo A, Rinfret S. Procedural and long-term outcomes of percutaneous coronary intervention for in-stent chronic total occlusion. Cardiovascular Interventions. 2017 May 8;10(9):892-902.
9. Dangas GD, Claessen BE, Caixeta A, Sanidas EA, Mintz GS, Mehran R. In-stent restenosis in the drug-eluting stent era. J Am Coll Cardiol 2010; 56: 1897-1907.
10. Karmpaliotis D, Hatem R. In-Stent CTO, Not as Easy as it Looks. JACC Cardiovasc Interv 2017; 10: 903-905.
11. Yoon YH, Lee PH, Lee SW, Kwon O, Lee K, Kang DY, et al. Clinical outcomes after percutaneous coronary intervention for in-stent chronic total occlusion. EuroIntervention 2020; 16: e472-e479.
12. Hong SJ, Kim BK, Shin DH, Kim JS, Hong MK, Gwon HC, et al. Usefulness of intravascular ultrasound guidance in percutaneous coronary intervention with second-generation drug-eluting stents for chronic total occlusions (from the Multicenter Korean-Chronic Total Occlusion Registry). Am J Cardiol 2014; 114: 534-540.