Abstract
Objective: To describe the clinical characteristics and nursing care of patients with prolonged open thoracostomy, and to evaluate the effectiveness of a short training program for nurses.
Methods: This study is an exploratory two-case series involving patients with open thoracostomy treated at the Department of Thoracic and Cardiovascular Surgery, Hue Central Hospital (March–August 2025). In addition, 20 nurses participated in a 90-minute training session on open thoracostomy care; their knowledge and skills were assessed before and after using a multiple-choice test and a structured skills checklist.
Results: In two representative cases, chest drainage volume decreased by more than 70%, pain scores were reduced by 50%, dyspnea improved by 1–2 grades on the mMRC scale, and wound infection was effectively controlled. Among nurses, mean knowledge scores improved markedly from 6.1±1.1 to 8.9±0.7 (p<0.001). All practical skill domains demonstrated significant post-training improvement, including preparation and safety, initial assessment, wound care with ventilation maintenance, respiratory monitoring, and supportive care (all p<0.001). Documentation and reporting showed a mild increase (0.6±0.5 to 0.9±0.3) but did not reach statistical significance, consistent with the fact that this task was already performed routinely at baseline.
Conclusion: Nurses play a crucial role in the care of patients with open thoracostomy. As an exploratory two-case series, these findings should be considered preliminary, offering early evidence that supports the initial development of a standardized nursing care protocol for open thoracostomy.
Keywords
Open thoracostomy, Nursing care, Infection control, Nurse education
Introduction
Open thoracostomy is a special surgical technique indicated in cases of late-stage empyema, ruptured lung abscess, or severe intrathoracic infection where closed drainage is not feasible. However, this procedure carries a substantial risk of complications. A prehospital study reported complications in 10.6% of cases, including iatrogenic injury, infection, and missed or recurrent tension pneumothorax [1]. In contrast, studies on closed tube thoracostomy have shown complication rates ranging from 6% to 37%, depending on the clinical context and underlying conditions [2,3]. Open thoracostomy is typically indicated in advanced empyema or complex pleural infections where thick pus, multiloculation, or a trapped lung prevent effective closed drainage. The open cavity directly exposes the pleural space to the external environment, increasing the risk of persistent infection, fluid and heat loss, impaired ventilation, and psychological distress. These factors make wound care, infection prevention, respiratory monitoring, and pain management uniquely challenging for nurses, who play a central role in maintaining patient stability throughout the prolonged drainage period.
At present, guidelines from the Ministry of Health and domestic nursing protocols mainly address closed chest drainage, with no standardized protocol specifically for open thoracostomy [4]. Similarly, classical nursing textbooks in surgery, internal medicine, and pediatrics only cover closed drainage, without dedicated content for open drainage [5,6].
Compared with closed thoracostomy—where reported complication rates range from 6% to 37%—open thoracostomy carries higher risks of prolonged drainage, periwound infection, and delayed recovery, underscoring the need for tailored and standardized nursing interventions. This gap in guidance is especially relevant in Vietnamese hospitals, where resource constraints and variability in nursing practice may further affect patient outcomes.
At the Department of Thoracic and Cardiovascular Surgery, Hue Central Hospital, we have encountered several cases requiring prolonged open thoracostomy—posing both clinical challenges and opportunities for experience-sharing. From this practical basis, we conducted a case series of two patients combined with a short training session for 20 nurses, with the aim of initiating the development of a standardized nursing care protocol tailored for open thoracostomy.
Study Population and Methods
Study population
- Patients: Two cases of prolonged open thoracostomy treated at the Department of Thoracic and Cardiovascular Surgery, Hue Central Hospital (June–August 2025).
- Inclusion criteria:
- Indication for open thoracostomy due to complicated pleural infection with thick pus or extensive adhesions.
- Duration of open drainage ≥ 14 days.
- Complete medical records with observable clinical data.
- Patient or family consent to participate in the report.
- Inclusion criteria:
- Nurses: Twenty nurses working in the department, directly involved in the care of patients with open thoracostomy.
Study design
- Case series: Description of clinical characteristics, progression, and nursing care of the two patients.
- Short training intervention: One 90-minute training session on open thoracostomy care for 20 nurses. Effectiveness was assessed using a multiple-choice knowledge test and a structured practical skills checklist before and after training.
- The 90-minute training session consisted of three components: (1) a 30-minute mini-lecture reviewing indications, risks, and nursing principles for open thoracostomy; (2) a 30-minute demonstration of aseptic dressing, respiratory monitoring, and complication recognition by a senior nurse educator; and (3) a 30-minute return-demonstration session in which participants practiced skills under supervision.
Study content
- Patients:
- Demographics: age, sex, comorbidities, diagnosis, indication for open thoracostomy.
- Wound status: site of opening, daily drainage volume, odor, condition of surrounding skin, pain level (VAS 0–10), dyspnea (mMRC 0–4), psychological cooperation.
- Nursing care protocol: preparation and safety, initial clinical assessment, wound care and maintenance of ventilation, respiratory monitoring and early detection of complications, supportive care and prevention measures, documentation and reporting.
- Outcomes: wound healing, infection control, pain level, respiratory function, patient cooperation.
- Nurses:
Knowledge and skills comparison before and after training, evaluated with a 10-item MCQ for knowledge test and 20-item skill checklist
Data collection and analysis
Patients:
- Data collected from medical records, nursing care sheets, and direct observation.
- Evaluation parameters:
- Demographics: age, sex, comorbidities, diagnosis.
- Wound status: site of opening, daily drainage volume (ml), odor, surrounding skin condition (inflammation, erythema, ulceration).
- Pain: visual analog scale (VAS, 0–10).
- Dyspnea: modified Medical Research Council (mMRC, 0–4).
- Psychological cooperation: anxious, fatigued, stable, cooperative.
- Timing: daily or periodically during the period of open thoracostomy until clinical improvement was achieved.
Nurses:
- Knowledge: 10-item multiple-choice test administered before and after the training session (score range 0–10). (Appendix 1).
- Skills: 20-item checklist on open thoracostomy care, evaluated before and after training (Appendix 2).
- Timing: immediately before and after the training session.
- Validity and reliability: The knowledge test and the 20-item skills checklist were reviewed independently by two senior thoracic surgery nurses and one thoracic surgeon for content relevance and clarity. Revisions were made based on their expert feedback to enhance content validity.
- During the skills assessment, two nurse educators jointly evaluated each participant’s return-demonstration. Scores were assigned through consensus to maintain consistency and reduce inter-rater variability.
Data analysis:
- Data entry and management using SPSS version 26.0 (IBM, USA).
- Descriptive statistics:
- Quantitative variables: mean ± standard deviation (Mean ± SD).
- Categorical variables: percentage (%).
- Comparisons before and after training:
- Quantitative variables (knowledge scores, skill scores): paired t-test; significance set at p<0.05.
- Results presentation: tables and bar charts comparing pre- and post-training scores, as well as drainage volume, pain, and dyspnea.
Ethics:
- The study was conducted in accordance with institutional and national ethical standards.
- All data were anonymized and used exclusively for research and quality improvement purposes.
- Written informed consent was obtained from patients or their legal representatives for participation and for the use of clinical information.
- Nurse participants were informed about the study purpose and provided verbal consent before completing the knowledge test and skills assessment.
Results
Case characteristics
General characteristics of the two cases are presented in Table 1.
|
Case |
Age/Sex |
Comorbidity |
Diagnosis & indication for open thoracostomy |
Duration of open drainage |
Initial complications |
|
1 |
54/M |
None |
Lung abscess ruptured into the pleural cavity |
21 days |
Severe pain, anxiety |
|
2 |
62/F |
None |
After pleural drainage for treatment of empyema |
35 days |
Heavy drainage, periwound infection |
Clinical progress after nursing care
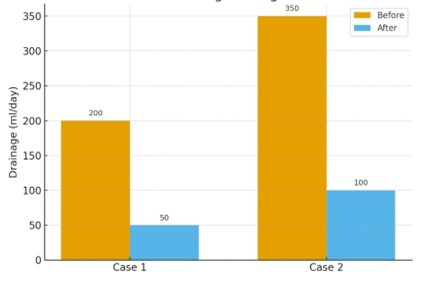
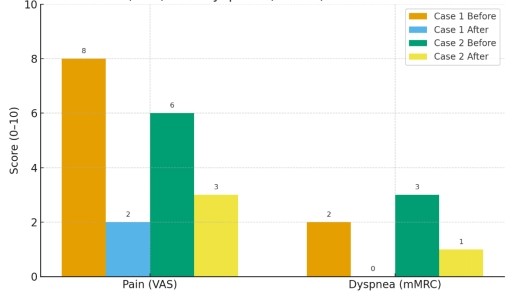
The outcomes of nursing care are presented in Table 2.
|
Indicator |
Case 1 |
Case 2 |
|
Daily drainage volume |
200 ml → 50 ml |
350 ml → 100 ml |
|
Pain (VAS) |
8/10 → 2/10 |
6/10 → 3/10 |
|
Dyspnea (mMRC) |
Grade 2 → 0 |
Grade 3 → Grade 1 |
|
Wound infection |
None → None |
Redness → Clean skin |
|
Psychological status/cooperation |
Anxiety → Stable |
Fatigue → Cooperative |
General evaluation: In both cases, drainage volume decreased by more than 70% (Figure 1), pain scores were reduced by ≥50%, dyspnea improved by 1–2 grades on the mMRC scale (Figure 2), wound infection was controlled, and psychological status became more stable.
Figure 1. Patient progression in volume drainage.
Figure 2. Patient progression in pain (VAS score) and dyspnea (mMRC score).
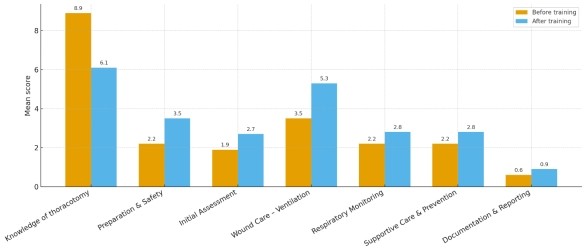
Nursing training outcomes
The outcomes of nursing training are presented in Table 3 and Figure 3.
Figure 3. Comparison of nurses’ knowledge and skills before and after training.
|
Evaluation item |
Before training (Mean ± SD) |
After training (Mean ± SD) |
p-value |
|
Knowledge of thoracotomy |
8.9±0.7 |
6.1±1.1 |
<0.001 |
|
Preparation and Safety |
2.2±0.6 |
3.50±0.5 |
<0.001 |
|
Initial Assessment |
1.9±0.6 |
2.7±0.5 |
<0.001 |
|
Wound Care – Ensuring Ventilation |
3.5±0.5 |
5.3±0.5 |
<0.001 |
|
Respiratory Monitoring |
2.2±0.6 |
2.8±0.4 |
0.002 |
|
Supportive Care and Prevention |
2.2±0.6 |
2.8±0.4 |
0.002 |
|
Documentation and Reporting |
0.6±0.5 |
0.9±0.3 |
0.055 |
Discussion
Central role of nursing
Recovery in patients with open thoracostomy depends not only on surgical intervention but also on continuous, meticulous, and timely nursing care. In the two reported cases, nurses played a pivotal role in wound dressing, infection control, drainage monitoring, respiratory support, and psychological stabilization. Clinical outcomes demonstrated a >70% reduction in drainage volume, ≥50% reduction in pain, 1–2 grade improvement in dyspnea, and effective infection control. These findings highlight that nurses act as the “safety gatekeepers” in the recovery process of patients with open thoracostomy.
Improvements in drainage volume, pain scores, and dyspnea were closely associated with targeted nursing interventions. Regular aseptic wound care and monitoring helped reduce periwound inflammation and infection, while consistent respiratory support and early mobilization contributed to improved mMRC scores. Pain assessment and timely administration of analgesia enabled better patient cooperation, which further facilitated effective drainage and wound healing.
Novelty of the study
In Vietnam, there have been virtually no formal publications describing a nursing care protocol specific to open thoracostomy. Existing guidelines and textbooks focus primarily on closed chest drainage [4–6]. Several international studies have emphasized the importance of nursing in preventing complications and reducing recovery time [7]. This report represents one of the first domestic pieces of evidence to describe in detail two cases of prolonged open thoracostomy, while also incorporating a short nursing training model that significantly improved knowledge and skills [8]. To our knowledge, this is the first structured report in Vietnam to systematize case-based nursing experience into training content and suggest a framework for protocol standardization [9].
Effectiveness of short-term training
Overall, the training program led to substantial improvements across nearly all domains, with mean scores increasing by 1–2 points in preparation, assessment, wound care, ventilation management, respiratory monitoring, and supportive care (all p<0.01). These improvements reflect enhanced confidence, better procedural consistency, and reduced hesitation when handling complex clinical situations.
Importantly, the Documentation and Reporting domain did not show a statistically significant change (p=0.055). This result is expected, as documentation practices were already well-established and routinely performed correctly before the training. Therefore, the lack of significant improvement simply indicates that nurses had already achieved a good baseline level in this administrative skill, leaving limited room for further measurable enhancement.
This supports the feasibility and effectiveness of short, focused training models, enabling nurses to feel more confident in managing complex cases such as open thoracostomy.
Urgency of protocol standardization
The absence of standardized guidelines means current nursing practice largely relies on personal experience, which increases the risk of errors and may prolong hospitalization. The combination of case reporting and short-term training not only produced immediate benefits but also laid the groundwork for developing standardized nursing care protocols for patients with open thoracostomy in Vietnam.
Globally, organizations such as the British Thoracic Society and the World Health Organization have emphasized structured nursing frameworks for chest drainage and wound care, highlighting the importance of standardized aseptic technique, complication surveillance, and patient education. Incorporating principles from these international guidelines supports the rationale for developing a context-appropriate standardized protocol for open thoracostomy in Vietnam.
Limitations and recommendations
- Limitations:
- Small scale: only two cases and 20 nurses.
- Lack of control group and short follow-up duration.
- Interpretation of the results should consider potential confounders, including variations in physician management such as antibiotic selection, timing of surgical debridement, and differences in initial disease severity. Additionally, the duration of illness prior to admission may have influenced recovery speed, independent of nursing interventions.
- Recommendations:
- Future studies should include larger samples and controlled intervention designs to validate effectiveness.
- A standardized nursing care protocol for open thoracostomy should be developed and gradually implemented across hospitals.
The training model based on representative clinical cases should be expanded to strengthen practice quality and nursing confidence.
Conclusion
This two-case report of prolonged open thoracostomy demonstrates the crucial role of nurses in patient care, infection control, and recovery support. Both cases showed marked clinical improvement in drainage reduction, pain relief, dyspnea, and infection control.
The short training program for 20 nurses significantly enhanced knowledge, skills, and confidence in handling complex clinical situations. This provides practical evidence and forms the foundation for developing standardized nursing care protocols for patients with open thoracostomy. Nurses serve as the safety gatekeepers, ensuring standardized and high-quality care for patients undergoing open thoracostomy. The findings from this exploratory two-case series highlight the need for broader, multi-center studies and support future efforts toward developing hospital-level and national nursing care protocols for open thoracostomy
???? Core message: “Nurses – the safety gatekeepers, practicing standardized care!”
Acknowledgements
The authors would like to express their sincere gratitude to MSc., MD. Nguyen Duc Dung – Head of the Department, MSc., MD. Nguyen Thuc, and MSc., MD. Vo Minh Tue from the Department of Thoracic and Cardiovascular Surgery, Hue Central Hospital, for their dedicated support, professional guidance, and valuable facilitation throughout the implementation and completion of this manuscript.
References
2. Kesieme EB, Dongo A, Ezemba N, Irekpita E, Jebbin N, Kesieme C. Tube thoracostomy: complications and its management. Pulm Med. 2012;2012:256878.
3. Baldt MM, Bankier AA, Germann PS, Pöschl GP, Skrbensky GT, Herold CJ. Complications after emergency tube thoracostomy: assessment with CT. Radiology. 1995 May;195(2):539-43.
4. Ministry of Health (Vietnam). Guidelines for Diagnosis and Treatment of Respiratory Diseases. Hanoi: Medical Publishing House; 2021.
5. Nguyen Thi Xuyen, Pham Thi Minh Duc. Internal Medicine Nursing. Hanoi: Medical Publishing House; 2018.
6. Nguyen Thi Xuyen, Pham Thi Minh Duc. Surgical Nursing. Hanoi: Medical Publishing House; 2019.
7. Laws D, Neville E, Duffy J; Pleural Diseases Group, Standards of Care Committee, British Thoracic Society. BTS guidelines for the insertion of a chest drain. Thorax. 2003 May;58 Suppl 2(Suppl 2):ii53-9.
8. Cant R, McKenna L, Cooper S. Assessing preregistration nursing students' clinical competence: a systematic review of objective measures. Int J Nurs Pract. 2013 Apr;19(2):163-76.
9. Hoan LT, Hoan LV, Linh TTK, Oanh NT, Nhi PT. Knowledge and skills in applying the nursing care process among intensive care nurses. Vietnam Medical Journal. 2024;541(3).