Abstract
Background: There were well-known racial/ethnic differences in colorectal cancer (CRC) screening in the United States (US).
Aims: To study the rate of CRC screening recommendation for individuals not up-to-date on screening and whether there were racial/ethnic differences in recommendation.
Data and Methods: All adults 50 to 75 years old in the 2021 National Health Interview Survey who were not up-to-date on CRC screening were included. The rate of CRC screening recommendation in the past 12 months was calculated for non-Hispanic Whites, Blacks/African Americans, Hispanics, and Asians respectively. Multivariate logistic regression was used to examine racial/ethnic differences in CRC screening recommendation, controlling for demographic and socioeconomic variables (age, sex, immigrant, college education and insured).
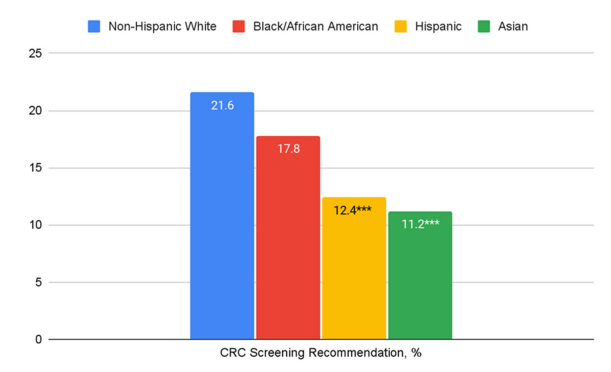
Results: Among the 3,363 individuals not up-to-date on CRC screening, the rate of CRC screening recommendation was low across all racial/ethnic groups (non-Hispanic Whites 21.6%, Blacks/African Americans 17.8%, Hispanics 12.4%, and Asians 11.2%). Compared with non-Hispanic Whites, CRC screening recommendation was significantly lower for Hispanics and Asians in multivariate logistic regression (Blacks/African Americans: odds ratio [OR] 0.82, 95% confidence interval [CI] 0.62-1.09; Hispanics: OR 0.66, 95% CI 0.47-0.93; Asians: OR 0.53, 95% CI 0.33-0.86), with other predictors including older age and uninsured.
Conclusions: The rate of CRC screening recommendation was low for individuals not up-to-date on screening, especially for Hispanics and Asians.
Introduction
In the United States (US), the rate of colorectal cancer (CRC) screening differs significantly by racial/ethnic group [1-3]. Some of the racial/ethnic differences may be related to differences in healthcare professional recommendation on CRC screening [4-6]. In this population-based study using the 2021 National Health Interview Survey (NHIS), we focused on individuals not up-to-date on CRC screening and studied screening recommendation by racial/ethnic group.
Data and Methods
The NHIS is the principal source of information on the health of the civilian noninstitutionalized population in the US (https://www.cdc.gov/nchs/nhis/index.htm). In the 2021 NHIS, CRC screening was defined as use of colonoscopy within 10 years, sigmoidoscopy within 5 years, CT (virtual) colonography within 5 years, ColoGuard within 3 years, or fecal occult blood test within 1 year.
Our study group included those individuals between 50 and 75 years old and not up-to-date on CRC screening. For these individuals, the 2021 NHIS specifically asked about CRC screening recommendation with the question “In the past 12 months, did a doctor or other health professional recommend that you be tested to look for problems in your colon or rectum?”. The demographic and socioeconomic variables of interest in the NHIS included age, sex, race/ethnicity, immigrant (vs. born in the US), college education, and insured (vs. uninsured).
The Student’s t-test and chi-square test were used in the statistical analysis of continuous and categorical variables respectively. We also used the multivariate logistic regression analysis to control for demographic and socioeconomic variables and examine the racial/ethnic differences in CRC screening recommendation.
Results
There was a total of 3,363 adults between 50 and 75 years old who were not up-to-date on CRC screening in the 2021 NHIS (Table 1). As expected, there were significant demographic and socioeconomic differences among racial/ethnic groups, with minorities slightly younger in age and much more likely to be immigrants, particularly Hispanics (64.8%) and Asians (89.3%) (both p<0.001 vs. non-Hispanic Whites). Compared with non-Hispanic Whites, Blacks/African Americans and Hispanics were less likely college educated and insured, while Asians were more likely college educated. The rate of CRC screening recommendation was universally low across all racial/ethnic groups (non-Hispanic Whites 21.6%, Blacks/African Americans 17.8%, Hispanics 12.4% [p<0.001 vs. non-Hispanic Whites], and Asians 11.2% [p<0.001 vs. non-Hispanic Whites]) (Figure 1).
|
Race/Ethnicity |
Non-Hispanic White |
Black/African American |
Hispanic |
Asian |
|
Number |
2276 |
387 |
458 |
242 |
|
Age, mean (standard deviation) |
60.2 (7.3) |
59.4 (7.0)* |
58.2 (6.9)*** |
58.2 (7.1)*** |
|
Female, % |
51 |
55.3 |
53.7 |
58.7* |
|
Immigrant, % |
7.5 |
16.3*** |
64.8*** |
89.3*** |
|
College, % |
45.3 |
31.8*** |
23.4*** |
55.4** |
|
Insured, % |
89.4 |
85.8* |
72.7*** |
88.4 |
| Notes: *p<0.05, **p<0.01, ***p<0.001 compared with non-Hispanic Whites. | ||||
Figure 1. Percentages of Colorectal Cancer (CRC) Screening Recommendation by Racial/Ethnic Group. Notes: ***p<0.001 compared with non-Hispanic Whites.
In multivariate logistic regression controlling for age and sex, CRC screening recommendation was significantly lower for Hispanics and Asians (Blacks/African Americans: odds ratio [OR] 0.78, 95% confidence interval [CI] 0.59-1.03; Hispanics: OR 0.51, 95% CI 0.38-0.68; Asians: OR 0.45, 95% CI 0.30-0.68) compared with non-Hispanic Whites (Table 2). These racial/ethnic differences in CRC screening recommendation remained significant but were smaller after additionally controlling for socioeconomic variables (Blacks/African Americans: OR 0.82, 95% CI 0.62-1.09; Hispanics: OR 0.66, 95% CI 0.47-0.93; Asians: OR 0.53, 95% CI 0.33-0.86), with age and insured also significant predictors of screening recommendation.
|
|
CRC Screening Recommendation |
CRC Screening Recommendation |
|
Age |
0.99 (0.98, 1.01) |
0.99 (0.98, 0.999)* |
|
Female |
1.07 (0.90, 1.27) |
1.02 (0.86, 1.22) |
|
Immigrant |
|
0.80 (0.60, 1.07) |
|
College |
|
1.00 (0.83, 1.19) |
|
Insured |
|
4.22 (2.80, 6.36)*** |
|
Race/Ethnicity (vs. non-Hispanic White) |
|
|
|
Black/African American |
0.78 (0.59, 1.03) |
0.82 (0.62, 1.09) |
|
Hispanic |
0.51 (0.38, 0.68)*** |
0.66 (0.47, 0.93)* |
|
Asian |
0.45 (0.30, 0.68)*** |
0.53 (0.33, 0.86)** |
| Notes: Numbers in each cell are odds ratio (95% confidence interval). *p<0.05, **p<0.01, ***p<0.001. | ||
Discussion
In this population-based study of adults 50 to 75 years old not up-to-date on CRC screening in the US in 2021, we found that less than a quarter of them were recommended screening by a healthcare professional in the past 12 months [13]. In addition, compared with non-Hispanic Whites, CRC screening recommendation was significantly lower in Hispanics and Asians even after controlling for demographic and socioeconomic variables [14-16]. Our study confirmed the importance of CRC screening recommendation by a healthcare professional in cancer prevention. Prevention strategies enhancing primary/preventive care access, in particular for Hispanics and Asians, will help reduce CRC morbidity and mortality in the US.
The main strength of our study is the use of a large, population-based survey in the US that inquired the use of all CRC screening tests and whether CRC screening was recommended by a healthcare professional in the past 12 months. We used multivariate regression analysis to control for demographic and socioeconomic variables and measured racial/ethnic specific differences in screening recommendation. On the other hand, we were limited by the nature of the NHIS, in particular the lack of detailed health information in order to exclude individuals with significant co-morbidities and not candidates for cancer screening. In addition, we could not ascertain the underlying reasons for lack of screening recommendation, potentially including but not limited to lack of access to primary/preventive care, language, financial, or transportation barrier, etc. Finally, the start of COVID pandemic might have reduced preventive care use in 2021.
In summary, among individuals not up-to-date on CRC screening in the US in 2021, more than three quarters were not recommended to undergo CRC screening by a healthcare professional in the past 12 months, especially for Hispanics and Asians. Improving primary/preventive care access, in particular for Hispanics and Asians, may help achieve the population goal of CRC prevention in the US.
Acknowledgments
No grant support and disclosure.
References
2. Siegel RL, Wagle NS, Cercek A, Smith RA, Jemal A. Colorectal cancer statistics, 2023. CA Cancer J Clin. 2023 May-Jun;73(3):233-54.
3. Sokale IO, Rosales O, Montealegre JR, Oluyomi AO, Thrift AP. Trends in Up-To-Date Colorectal Cancer Screening Among U.S. Adults Aged 50-75 Years and Variations by Race/Ethnicity and U.S. Census Bureau Divisions. AJPM Focus. 2022 Dec 10;2(1):100055.
4. Jerant AF, Fenton JJ, Franks P. Determinants of racial/ethnic colorectal cancer screening disparities. Arch Intern Med. 2008 Jun 23;168(12):1317-24.
5. May FP, Almario CV, Ponce N, Spiegel BM. Racial minorities are more likely than whites to report lack of provider recommendation for colon cancer screening. Am J Gastroenterol. 2015 Oct;110(10):1388-94.
6. Kane WJ, Fleming MA 2nd, Lynch KT, Friel CM, Williams MD, Hedrick TL, et al. Associations of Race, Ethnicity, and Social Determinants of Health With Colorectal Cancer Screening. Dis Colon Rectum. 2023 Sep 1;66(9):1223-33.
7. Torre LA, Sauer AM, Chen MS Jr, Kagawa-Singer M, Jemal A, Siegel RL. Cancer statistics for Asian Americans, Native Hawaiians, and Pacific Islanders, 2016: Converging incidence in males and females. CA Cancer J Clin. 2016 May;66(3):182-202.
8. Ma GX, Shive S, Tan Y, Gao W, Rhee J, Park M, et al. Community-based colorectal cancer intervention in underserved Korean Americans. Cancer Epidemiol. 2009 Nov;33(5):381-6.
9. Carney PA, Lee-Lin F, Mongoue-Tchokote S, Mori M, Leung H, Lau C, et al. Improving colorectal cancer screening in Asian Americans: Results of a randomized intervention study. Cancer. 2014 Jun 1;120(11):1702-12.
10. Nguyen BH, Stewart SL, Nguyen TT, Bui-Tong N, McPhee SJ. Effectiveness of Lay Health Worker Outreach in Reducing Disparities in Colorectal Cancer Screening in Vietnamese Americans. Am J Public Health. 2015 Oct;105(10):2083-9.
11. Inadomi JM, Issaka RB, Green BB. What Multilevel Interventions Do We Need to Increase the Colorectal Cancer Screening Rate to 80%? Clin Gastroenterol Hepatol. 2021 Apr;19(4):633-45.
12. Oh KM, An K, Lee M, Shin C, Steves SL. Colorectal cancer screening disparities in Asian Americans: the influences of patient-provider communication and social media use. Cancer Causes Control. 2023 Sep;34(9):813-27.
13. Bayly JE, Trivedi S, Mukamal KJ, Davis RB, Schonberg MA. Limited English proficiency and reported receipt of colorectal cancer screening among adults 45-75 in 2019 and 2021. Prev Med Rep. 2024 Feb 4;39:102638.
14. Gilbert A, Kanarek N. Colorectal cancer screening: physician recommendation is influential advice to Marylanders. Prev Med. 2005 Aug;41(2):367-79.
15. Jih J, Nguyen MP, Ly I, Tsoh JY, Le GM, Woo K, et al. The Role of Physician Recommendation in Colorectal Cancer Screening Receipt Among Immigrant Chinese Americans. J Immigr Minor Health. 2018 Dec;20(6):1483-9.
16. Finney Rutten LJ, Parks PD, Weiser E, Fan C, Jacobson DJ, Jenkins GD, et al. Health Care Provider Characteristics Associated With Colorectal Cancer Screening Preferences and Use. Mayo Clin Proc. 2022 Jan;97(1):101-9.